Experts Matter. Find Yours.
Search experts on 50,000+ topics. Or browse by topic category.
- Recent Searches
Connecting credible expert sources & academic research
ExpertFile is a trusted resource for journalists, industry, funding agencies and government policymakers looking for fresh perspectives and innovative academic research.









Spotlights
Read expert insights on a wide variety of topics and current events.
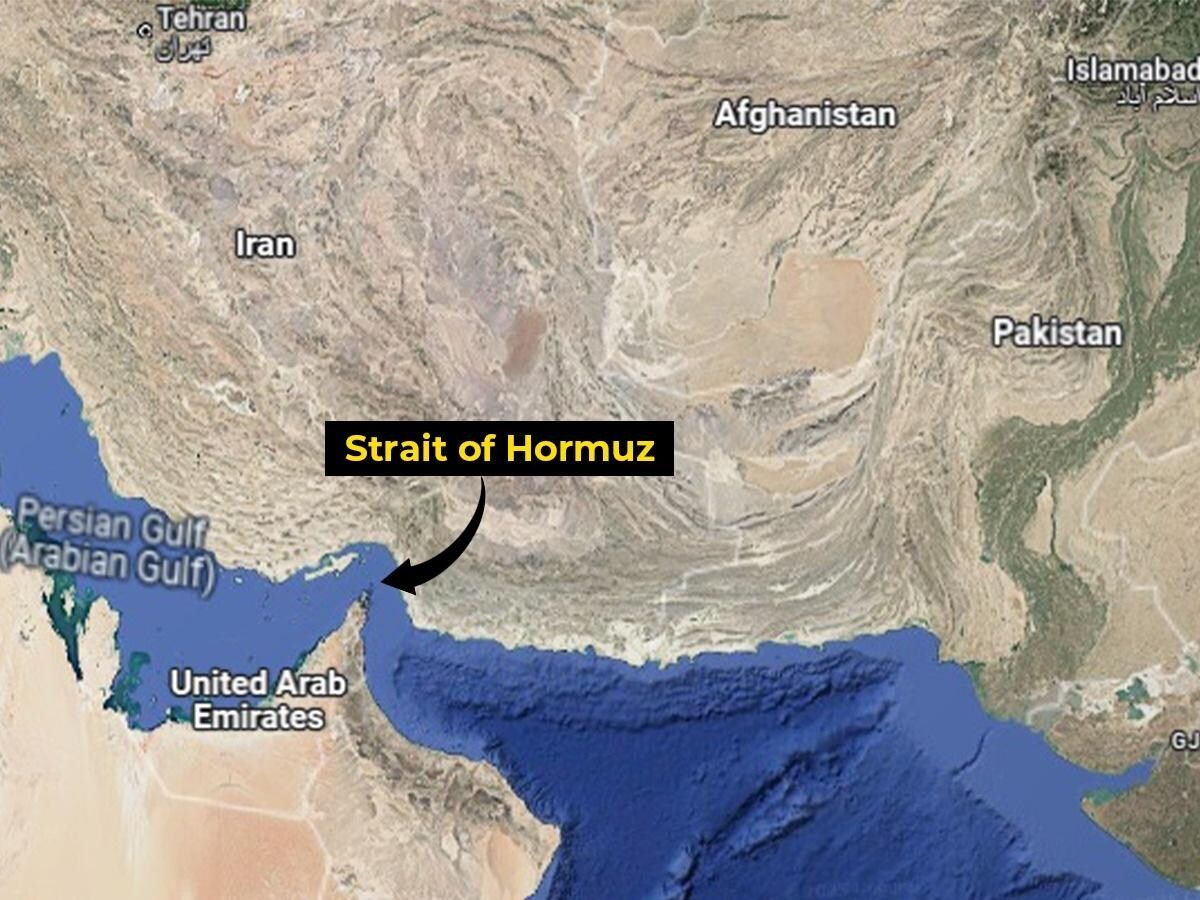
ExpertSpotlight: Why the Strait of Hormuz Matters: The World’s Most Critical Chokepoint
The Strait of Hormuz is one of the most strategically vital waterways on Earth. Just 20 miles wide at its narrowest point, with shipping lanes only a few miles across in each direction, this narrow channel connects the Persian Gulf to the Gulf of Oman and the Arabian Sea. Through it flows roughly one-fifth of the world’s petroleum supply, along with vast quantities of liquefied natural gas, particularly from Qatar. For global markets, the Strait is more than geography, it is a pressure point. Any disruption, even the threat of one, can send oil prices surging and rattle financial markets worldwide. A History Shaped by Empire and Energy For centuries, the Strait served as a maritime corridor linking Mesopotamia, Persia, India, and East Africa. Control over it shifted between regional powers, colonial empires, and eventually modern nation-states. In the 16th century, the Portuguese seized nearby islands to dominate regional trade routes. Later, British naval power asserted influence during the height of imperial shipping dominance. In the 20th century, however, the Strait’s importance expanded dramatically with the rise of oil exports from Gulf states. After the 1979 Iranian Revolution, tensions surrounding the Strait intensified. During the Iran-Iraq War in the 1980s, particularly the so-called “Tanker War” phase, commercial vessels were targeted, highlighting how vulnerable global energy supplies could be. Since then, periodic confrontations between Iran, the United States, and regional powers have kept the Strait at the centre of geopolitical risk. Why It Is So Important Today 1. Energy Security Major oil producers including Saudi Arabia, Iraq, the UAE, Kuwait, and Qatar rely heavily on this route. Even short-term closures could disrupt millions of barrels per day in global supply. 2. Global Economic Stability Because oil is globally traded and priced, disruptions in the Strait impact fuel costs, inflation, shipping, and consumer prices worldwide — including in North America and Europe. 3. Military Strategy The Strait is bordered primarily by Iran to the north and Oman to the south. Iran has periodically threatened to close the passage in response to sanctions or military pressure. The U.S. Navy and allied forces maintain a consistent presence to ensure freedom of navigation. 4. Modern Geopolitical Flashpoint Recent decades have seen drone seizures, tanker detentions, and naval standoffs. Each incident reinforces how fragile global energy logistics can be when concentrated in a single corridor. The Strait as a Symbol of Interdependence The Strait of Hormuz underscores a central truth of globalization: the world’s economies are deeply interconnected and geographically vulnerable. A narrow stretch of water in the Middle East can influence gasoline prices in Ontario, manufacturing costs in Germany, and energy security debates in Asia. It is both a trade artery and a geopolitical lever — a reminder that geography still shapes global power. Expert Angles for Media An expert in geopolitics, energy economics, or maritime security could explore: How vulnerable is the global economy to a prolonged closure? Can alternative pipelines realistically replace Hormuz traffic? What role do regional alliances play in deterring conflict? How does the Strait shape Iran’s negotiating power? What would insurance and shipping markets do in a crisis? The Strait of Hormuz is not simply a map feature — it is one of the world’s most consequential strategic chokepoints. Its stability underpins global energy flows, economic predictability, and international security. If tensions rise there, the world feels it. Our experts can help! Connect with more experts here: www.expertfile.com
Surgery past 65? Brain health screening can aid recovery
Before surgery, your doctor will order evaluations to identify any health problems that may need to be addressed before the procedure. This typically includes medical histories, laboratory tests and checking blood pressure, heart rate and temperature. There’s one vital sign that is often not on the list, but is crucial for older adults: screening for mental and cognitive health. “There is an overwhelming amount of evidence that presurgical brain health predicts complications after surgery,” said Catherine Price, Ph.D., a professor in the University of Florida College of Public Health and Health Professions Department of Clinical and Health Psychology and the UF College of Medicine Department of Anesthesiology. “For example, individuals with weaknesses in memory and attention and people with neurodegenerative diseases, such as Parkinson’s, have higher rates of confusion and memory complications that affect their recovery from surgery.” Research by Price and others has shown that a patient’s cognitive, memory and mental health status before surgery is an excellent indicator of whether they will experience cognitive problems such as delirium, a common complications in older adults after surgery. Delirium, characterized by confusion, disorientation and impaired awareness, can lead to longer recovery times, increased dementia risk, higher mortality rates and health care costs. Price founded and directs the University of Florida Perioperative Cognitive Anesthesia Network, or PeCAN, a first-of-its-kind, multidisciplinary program that seeks to identify older adults who may be at risk of developing cognitive problems after surgery so that clinicians can intervene. In recent findings published in the journal Anesthesia and Analgesia, Price and her colleagues report on two years of PeCAN patient data. Of the thousands of patients over age 65 who received presurgical screening, 23% were found to have issues with their cognitive performance, yet only 2% of the patients screened had a previous note in their medical charts indicating they had a cognitive impairment. “It’s so important to know when an individual has cognitive complications because that changes their care path,” Price said. “From medication to monitoring, the patient’s care is more complex for the perioperative team and family.” For PeCAN patients identified as being at risk for postsurgery cognitive problems, Price and her team will share tailored recommendations with the patient’s care team before, during and after surgery. These may include more monitoring during anesthesia and medication adjustments, such as using medications for nausea and pain management less likely to contribute to delirium. The PeCAN team also might offer the surgical care team specific communication strategies. For example, health care providers should repeat information several times for patients who have trouble remembering new material and ask them to write it down. Recently published research by Price and colleagues found PeCAN patients reported the focus on brain health improved confidence in their surgical team and care plan. Health care systems are only starting to incorporate preoperative brain health teams like PeCAN. Until they are offered more frequently, Price offers a few steps anyone can take to help protect brain health, including a focus on reducing inflammation in the body prior to surgery. To help achieve this: Optimize nutrition. Reduce your intake of added sugars and refined carbohydrates, like white bread. Get good sleep. Improve sleep hygiene so you are well-rested. “Sleep is essential for the brain for a number of reasons,” Price said. Reduce alcohol intake to limit inflammation and dehydration. Pay attention to your medications. Follow your care team’s instructions. Enlist a family member or caregiver to help you keep tabs on what you’re taking, how much and how often. Practice techniques to limit anxiety, such as visualization and deep breathing. The box breathing method is an easy one to remember: Breathe in slowly for four seconds. Hold your breath for four seconds. Slowly exhale for four seconds. Wait four seconds before inhaling again.

Got Expertise to Share?
Join leading professionals already using ExpertFile’s easy to use Platform for showcasing your organization’s experts and their insights on your website...and to the world.
Solving for X: Expert highlights importance of algebra in middle and high school
Math educators agree that Algebra is a critical course for middle and high schoolers, often serving as a gateway to more advanced math courses and influencing students’ academic trajectories in STEM pathways. Yet, many students struggle in this important course. Since May 2025, University of Delaware Associate Professor Erica Litke has partnered with the University of Pennsylvania Graduate School of Education and the School District of Philadelphia in a $5 million, three-year initiative to improve algebra teaching in the district. The project offers algebra teachers professional development through a year-long fellowship. With expertise in improving instructional quality in math and supporting algebra teaching, Litke leads the design and delivery of the professional development with Penn GSE experts. Close to 80 teachers participated in the first cohort of the fellowship, which includes a four-day summer institute. Litke’s research in math education has connected instructional quality to broader policy issues in education and focused on teacher knowledge and professional development. “The focus on algebra content and key features of algebra teaching that support students in learning algebra content helps teachers translate their learning from the fellowship directly into their teaching practice,” said Litke. “Being able to translate my research findings into usable knowledge for teachers and contribute to the design of this kind of comprehensive professional learning has been really exciting.” Litke can speak to her role in the Algebra Fellowship project, the importance of Algebra 1 in the trajectory of students’ STEM education and strategies for supporting teaching learning at the school and district levels. ABOUT ERICA LITKE Erica Litke is an associate professor specializing in mathematics education in the School of Education at the University of Delaware. Her research focuses on understanding and improving instructional quality in mathematics for students in the elementary and secondary grades. Her research has described and analyzed instructional practice in mathematics using observation instruments, connected instructional quality in mathematics to broader policy-related issues in education, and focused on teacher knowledge and professional development. She has appeared in The Philadelphia Inquirer, Daily Pennsylvanian and other publications. To speak with Litke or to learn more, email mediarelations@udel.edu.

Florida renters struggle with housing costs, new statewide report finds
Nearly 905,000 low-income renter households in Florida are struggling to afford their housing costs, according to the 2025 Statewide Rental Market Study, released by the University of Florida’s Shimberg Center for Housing Studies. Prepared for Florida Housing Finance Corporation, the report provides a comprehensive look at the state’s rental housing conditions and is used to guide funding decisions for Florida Housing’s multifamily programs, including the State Apartment Incentive Loan (SAIL) program. “Florida’s strong population growth has collided with limited housing supply, pushing rents beyond what many families can afford,” said Anne Ray, manager of the Florida Housing Data Clearinghouse at the Shimberg Center. “This report helps policymakers and housing providers target resources where the need is most acute — including communities that are experiencing the fastest growth and the greatest affordability gaps.” Key findings from the 2025 study include: A growing affordability gap: An estimated 904,635 renter households earning below 60% of their area median income (AMI) are cost burdened, paying more than 40% of their income toward rent. These households are spread across the state, with 64% in Florida's nine most populous counties, 33% in mid-sized counties and 3% in small, rural counties. Surging population and higher rent and housing costs: Between 2019 and 2023, Florida added more than 1 million households — nearly 195,000 of them renters — driven by in-migration from states like New York, Illinois and California. Despite the addition of more than 240,000 multifamily units, median rent soared nearly $500 per month, from $1,238 to $1,719. After years of growth, Florida's older renter population is holding steady: Renters age 55 and older represent 39% of cost burdened households, up from 29% in 2010 but similar to 2022 numbers. Most renters are working: 79% of renter households include at least one employed adult, compared to 67% of owner households. Most non-working renters are seniors or people with disabilities. Homelessness is on the rise: The report estimates 29,848 individuals and 44,234 families are without stable housing, up from 2022, as hurricanes and tight markets contribute to displacement. Assisted housing provides an alternative to high-cost private market rentals: Developments funded by Florida Housing, HUD, USDA and local housing finance authorities provide over 314,000 affordable rental units statewide. Future risks to affordable housing stock: More than 33,000 publicly assisted units may lose affordability protections by 2034 unless renewed. Evalu ating affordable housing in Florida “State- and federally-assisted rental housing developments are essential to providing stable, affordable homes for Florida’s workforce, seniors, and people with special needs,” Ray said. “Florida Housing Finance Corporation’s programs make up a significant portion of this housing, and our study helps ensure those resources are directed where they’re needed most. Preserving these developments — and expanding them — is critical to keeping pace with Florida’s growing population and maintaining affordability.” Since 2001, the Shimberg Center has produced the Rental Market Study every three years to inform strategic investments in affordable housing across Florida. The study evaluates needs across regions and among key populations including seniors, people with disabilities, farmworkers and others. The Rental Market Study and the Florida Housing Data Clearinghouse are part of a 25-year partnership between the Shimberg Center and Florida Housing Finance Corporation to support data-driven housing policy and planning.

The science behind the blood moon: Understanding this lunar phenomenon ahead of march's event
March's celestial event – a blood moon – is just around the corner. This captivating lunar spectacle isn't just a cool sight to behold; it has some neat science backing it up. The blood moon phenomenon happens during a total lunar eclipse. "During a total lunar eclipse, the only light that reaches the surface of the moon is refracted through the Earth's atmosphere, which essentially acts like a lens. Light is a wave, and every color of the rainbow has a different wavelength – red the longest and violet the shortest," said Bennett Maruca, associate professor of physics and astronomy at the University of Delaware. What adds to the excitement is the rare nature of total lunar eclipses. While partial eclipses occur more frequently, a full blood moon isn't an everyday event. Depending on where you live, the blood moon may only grace the night skies a few times a decade. "One of my favorite things about total lunar eclipses is that it's hard to know ahead of time quite what it will look like. The moon can take on a color ranging from burnt orange to red to grayish brown," he said. "The closer the Moon passes to the center of Earth's shadow, the darker the color will be." Maruca is available to speak about the event, which takes place in the wee hours of March 3. He can discuss when to wake up to see the phenomenon and how to best capture it. "For photographing the moon, I would recommend a camera with some optical zoom – the moon is only about 0.5 degrees across. Because of the low lighting conditions, a tripod or other support would be helpful since a longer exposure time will be needed," he noted. He has appeared in a number of outlets including Mashable and The Philadelphia Inquirer. He can be contacted by clicking on his profile. ABOUT BENNET MARUCA Bennett Maruca serves as an associate professor in the University of Delaware's department of physics and astronomy. His research focuses on the sun, the solar wind and other space plasmas. He is a recipient of the Antarctic Service Medal and NASA's Silver Achievement Medal. He also serves as an associate director of the Delaware Space Grant Consortium and is currently mentoring over twenty undergraduate students developing experiments to fly into space to observe Earth's ionosphere.

The truth behind federal disclosure of alien life
With the recent presidential comments on potential alien life, UFO enthusiasts have new hope that finally we’re going to get federal “disclosure” of UFOs, aliens and the great government conspiracy surrounding both. But, as a scientist who studies the search for life in the Universe, the question I have is much simpler: What would disclosure really need to disclose? What is required for actual, factual proof that aliens exist and they’ve been visiting Earth? We’ve already had three years of Congressional hearings on UFOs that have produced zero proof of anything. What we need now is simple: hard physical evidence. That is what disclosure needs to deliver. Not stories about alien spaceships being held by the government, but the actual spaceships themselves. Not stories about alien bodies but the actual icky, gooey bodies with their icky gooey tentacles. If disclosure provides physical evidence that independent laboratories and independent scientists all over the world can verify, then it will live up to its hype. That would make “Disclosure Day” truly history-making.

Laura Mauldin's rule of thumb is that if you think you're caregiving, you probably are. The University of Connecticut professor and author has a new book that just been released In Sickness and in Health, where an urgent argument is made that America’s caregiving crisis is not a private family matter, but a structural and political failure. Mauldin isn't just a scholar in the field. She also speaks from personal experience about the impact of caregiving -- as well as how society views and values it -- on both caregivers and those that they care for. It may not have been the birthday present then 32-year-old Laura Mauldin wanted to buy herself, but purchasing long-term care insurance was something she knew she needed. Mauldin, an associate professor in UConn’s Department of Social and Critical Inquiry, had been caring for her sick partner the five years prior, watching as cancer destroyed the promise of a long life. “It’s not about being morbid, rather it’s about recognizing the inevitability of a completely typical, expectable part of life,” Mauldin says of her advanced planning. “Why not just go ahead and in a neutral way have a plan? Then it’s there, you don’t have to worry, and you can feel more prepared.” A detailed account of her caregiving experience is the launching point for her new book, “In Sickness and in Health,” released this month by HarperCollins’ Ecco Press, in which she tells the story of a handful of couples from around the country who she came to know over years of spending time with them, oftentimes days and nights. “I grew to love these people and to care about them,” she says. “Their stories tell us something bigger about our culture, about our society, and about our choices around care policy and care systems. Theirs are the hidden stories that are going on behind millions of closed doors.” In her quest to bring discussions about caregiving to the light of day, Mauldin sat with UConn Today recently to talk about the different forms that caregiving can take, the result of absent social safety nets, and how ableism permeates the culture. February 2026 - UConn Today Drawing from her new book, Mauldin blends her personal experience with sociological research to show how love, marriage, and devotion are routinely forced to compensate for weak public policy, limited Medicaid support, and a culture shaped by ableism. Her work reframes caregiving as essential labor, deeply gendered, largely invisible, and profoundly political, and challenges the notion that “love is enough” in a system that offers far too little support. It’s an old adage: when people get married, they promise to stick together “in sickness and in health.” But that’s easier said than done when you’re caregiving for a spouse or long-term partner, when systemic failures often lead to burnout. In her new book, In Sickness and in Health: Love Stories from the Front Lines of America’s Caregiving Crisis, University of Connecticut professor Laura Mauldin explores the relationships between caregivers and their disabled and sick spouses, and the underlying lack of structural support in the US that makes unpaid care an inescapable feature of most such relationships. The topic is personal for her: Maudlin’s partner’s leukemia came out of remission as they were getting closer in 2006. “Falling in love with J had called upon me to increasingly fill a role that required meeting nearly every one of her needs,” Mauldin writes in her introduction. “This was more than just providing emotional support when the person you love is suffering.” J passed away in 2010. I spoke to Mauldin about crafting this book based on her lived experiences, how systems fail both disabled people and their caregivers, and what is at stake with Medicaid cuts exacerbating the damage to an already broken system. February 2026 - Mother Jones Dr. Laura Mauldin, an associate professor in the Department of Social and Critical Inquiry at the University of Connecticut, blends rigorous scholarship with lived experience to challenge prevailing assumptions about caregiving, disability, and public policy. Her work exposes how cultural norms and policy gaps intersect to offload care onto private homes, obscuring the true costs of care and the human toll of under-resourced support systems. She is available to speak with media - simply click on her icon now to arrange an interview today.

Expert Q and A: Understanding "Punch," The Baby Monkey That Captured The World's Heart
A tiny Japanese macaque named Punch has unexpectedly become one of the internet’s most talked-about animals. Born at a zoo in Japan and rejected by his mother shortly after birth, the young monkey was hand-raised by staff and given a stuffed toy for comfort—an image that quickly ricocheted across social media worldwide. Videos showing Punch tentatively approaching other macaques, sometimes being pushed away or corrected as he tried to socialize, struck an emotional chord. What began as a local zoo update rapidly turned into international headlines, with audiences from North America to Europe weighing in on what they saw as loneliness, resilience and the universal need for belonging. But experts say the story is more nuanced than a viral clip suggests. The interactions that many viewers interpreted as bullying are, in fact, typical components of macaque social development, part of how young primates learn boundaries, hierarchy and group norms. While Punch’s early maternal separation makes his integration more delicate, gradual acceptance into the troop is a positive sign. As internet users continue to share and comment, the moment has sparked broader conversations about animal emotion, anthropomorphism and the realities of wildlife behavior in managed care settings. Florida Tech's Catherine Talbot offered insight into the complexities of animal behavior. Catherine F. Talbot is an assistant professor in the School of Psychology at Florida Tech and co-director of the Animal Cognitive Research Center at Brevard Zoo. Her overarching research goal has been to study the ultimate (evolutionary) and proximate (behavioral, biological, and developmental) mechanisms underlying sociality. Q: Is it normal for mother macaques to abandon their babies, or is this an unusual occurrence? What circumstances can cause this to happen? It’s not necessarily normal, but also not that uncommon in primates, unfortunately. It’s more common in first time mothers that are inexperienced and sometimes lower ranking mothers. A number of factors can increase the likelihood of abandonment including stress on the mother and unfavorable conditions such as limited resources. Q: How does abandonment affect development in young macaques? Early maternal contact is critical for normal behavioral and emotional development. Infants rely on their mothers for nutrition, warmth, protection and learning how to navigate social dynamics. When infants do not have their mothers during critical developmental periods like infancy, in the short term, they tend to have elevated stress responses and difficulty with emotional regulation. In the long-term, it depends on whether the infant is able to form other types of attachment. In the worst-case scenario, they may have increased aggression, abnormal and/or self-injurious behavior, digestive issues and may lack social skills. But primates are resilient, and with social support and gradual integration into a troop, Punch can form new attachments, learn socially appropriate behavior and ultimately live a fairly normal monkey life. Q: Is it obvious to the rest of the troop when a young macaque has no mother? How does this affect integration? Japanese macaques have really complex social worlds, so they are really in tune with the relationships they have with one another and recognize the relationships between other individuals. That can certainly make it more difficult for Punch to be accepted back into the troop – he needs to find some friends and possibly even a surrogate parent. With social support, he should be able to recover from the absence of a mother. It’s really great to see that the care staff stepped in to support Punch as he begins to recovery from the stress of this experience. It’s even more important that Punch is around other monkeys of the same species so that he can continue to learn from them and respond appropriately to social communication cues. I’m thrilled to see that Punch is now making friends. Q: Punch is obviously attached to his stuffed orangutan. We can understand how this happens from our own human experience, but can you explain, on a biological level, how he bonded with this stuffed animal? Primates, including humans, are neurobiologically wired to form strong social bonds with a caregiver very early in life. In many primate species, infants are born highly dependent on their mother. Punch’s attachment to the stuffed orangutan reflects this need for attachment. That physical touch – warmth, softness, graspable limbs, a stable physical presence – can partially activate those same calming biological pathways, including the release of oxytocin which regulates stress and promotes feelings of safety. Without activation in those pathways, Punch would likely experience stronger feelings of separation or loneliness and ultimately social withdrawal. These biological pathways are crucial to proper social and emotional development of any primate species. Any way we can help mitigate those effects for Punch is crucial for successful integration back into his troop. Q: How does sociality among Japanese macaques compare to that of similar species? Japanese macaques live in large multi-male, multi-female social groups that can range from roughly 50 to 150 individuals. Like many macaques species, they form stable, female-bonded societies. Females remain in their natal group (or the group they were born into) for life, inherit their mother’s rank, and form strong kin- based alliances whereas males emigrate to a new group at adolescence. Their societies are organized around matrilines or extended female family lines in which rank is very important. They have strong dominance hierarchies and generally high levels of aggression, but levels of aggression and tolerance can vary a good amount from group to group. Entire matrilines can outrank others, which dictates access to food, grooming partners, and coalitions. Within a single troop, you often see multiple matrilines with long-standing dominance competitions. I sometimes compare it to a Romeo and Juliet-style Montague and Capulet dynamic, where beneath the surface of daily grooming and foraging is a complex political landscape structured by kinship and status. Q: What behaviors can Punch expect from the rest of the monkeys as he continues to integrate with the troop? What behaviors can the troop expect to see from him? As Punch continues to integrate into his troop, I would expect to see some social testing by other members of the group to see how Punch responds- they may use mild aggression like open mouth threats or direct stares (which arethreatening is macaques), brief chases, and displacement from resources like food/resting spots. These will help clarify Punch’s rank and help form and maintain a stable hierarchy. Therefore, I hope to see Punch make at least a few strong social bonds (friends), to help defend him against more intense aggression. As long as he makes a few friends, he should begin to receive more affiliative behavior. Integration is usually gradual as these bonds form and strengthen and these skills develop. I would expect to see more play and grooming with conspecifics and less reliance on his stuffed orangutan as real social bonds start to form. Grooming is especially important for forming and maintaining social bonds and there are already videos showing Punch receiving some grooming from older monkeys, which bodes well for him. He also needs to respond in socially appropriate ways, like grooming others and showing submission to higher ranking individuals. Essentially, he needs to understand and follow the rules of Japanese macaque society. Q: What message do you have as people continue to root for Punch? It's uplifting to see how much support Punch has gained across the world. And while Punch is clearly adorable and so vulnerable that you just want to love him and give him (or other monkeys like him) a home, it’s important to remember that more than anything else, he needs to live with other monkeys so that he can live a life that is true to his species and nature. Unfortunately, many people still have monkeys as pets. The illegal wildlife trade is a multi-billion-dollar industry, ranking as the fourth largest illegal trade after drugs, arms, and human trafficking. Within the United States, it is estimated that there are more than 15,000 nonhuman primates living in unsuitable conditions. Primates are intelligent, sentient beings that need complex communities and relationships to thrive. There currently is no federal legislation that protects primates from private ownership, but the Captive Primate Safety Act (H.R.3199/ S.1594) has been proposed to prohibit the private possession of nonhuman primates and the sale or transportation of nonhuman primates for the wild pet trade. If you're interested in connecting with Catherine and learning more about animal behavior, let us help. Contact Adam Lowenstein, Assistant Vice President for External Affairs at Florida Institute of Technology, at adam@fit.edu to arrange an interview today.

Target Market: Who Are They, What Do They Value, and Where Are They?
In last week’s column on Super Bowl ads, I stressed the importance of providing a value proposition when you are advertising or marketing your goods and services. As a reminder, a value proposition is a promise that you make to potential customers that provides them a compelling reason why they should buy your product rather than a product from one of your competitors. Prior to developing a value proposition, you first need to understand who you are trying to sell to and what product characteristics they value. This will ensure that your value proposition will be more likely convince these buyers (your target market) to buy from you. The most effective Super Bowl ads from last week did this important work well. Once the company has a good, valuable proposition, it then needs to communicate that valuable proposition to its target market. Fortunately for companies with Super Bowl ads, just about all target markets are watching the game. However, for pretty much all other advertising and marketing, it must communicate where the target market will see or hear it. In today’s column, I will walk you through how to determine who your target market is, what they value, and finally, where to distribute your marketing messages. You are probably asking yourself, why is a guy who teaches Operations and Supply Chain Management (O&SCM) writing about Marketing? The answer is simple, really. It is the job of the O&SCM function of the company to deliver on the value proposition. So, as marketing develops its value proposition, it must confer with O&SCM to determine if the firm can deliver on that value proposition. If marketing communicates a value proposition it cannot meet, the company will likely be unsuccessful. With that in mind, let us examine the target market/value proposition development process. As a firm begins to identify its target market for a particular product, it must first determine the various potential customers who might buy that product and attempt to partition those customers into groups who value similar things. For instance, looking at the automobile market, there are some customers who value low price most, some who value performance and aesthetics most, and others who value reliability, durability, and consistency. If we are either in the automobile market or thinking about entering the automobile market, we need to find a group that values some characteristics that we think we can provide better than other market entrants. As you can see, the identification of a target market and the development of a value proposition that will appeal to that target market are done concurrently and iteratively. As noted above, the O&SCM function of the company is also brought in during these iterations to determine if the physical good can be manufactured or a service can be delivered in such a way that it can meet the value proposition. One important thing to remember is that in most cases, you are not your target market. What I mean by that is that you are often biased by your own knowledge and taste/preferences, and this may differ significantly from what your target market values. Remember that you are a unique individual whose preferences for a price point and evaluation of other characteristics might differ from your target market. Be sure to develop a value proposition that reflects the buying habits of your target market customers. Once you have developed a strong value proposition that you know your O&SCM can deliver upon, it is time to message that value proposition in places where your target market is present. As noted above, this aspect of our process is like “shooting fish in a barrel” for Super Bowl advertisers because all target markets are typically watching the Super Bowl. It is not so trivial for the rest of us. We need to understand what forms of media our target markets consume (e.g., television, radio, social media), but also, with each of these media, which applications or types of shows do they frequent. While most think social media skews young, and that is true for the most part, Facebook skews older, while Instagram, Snapchat, and TikTok skew much younger. On television, much of network television skew older, but there are shows like “Dancing with the Stars” and The “Bachelor” that do particularly well with younger women. Many mornings when I am getting ready for the day, I listen to “Augusta’s Morning News” on WGAC radio, and it is clear that my fellow listeners are primarily in my age demographic. My advice is to do your homework and find out where your target market is consuming media. All the work above is not very easy, but doing it right will lead to big returns. If you can identify who you want to target, based on what they value, and then be sure they get the marketing message that you have what they value, your business will succeed!