2 min
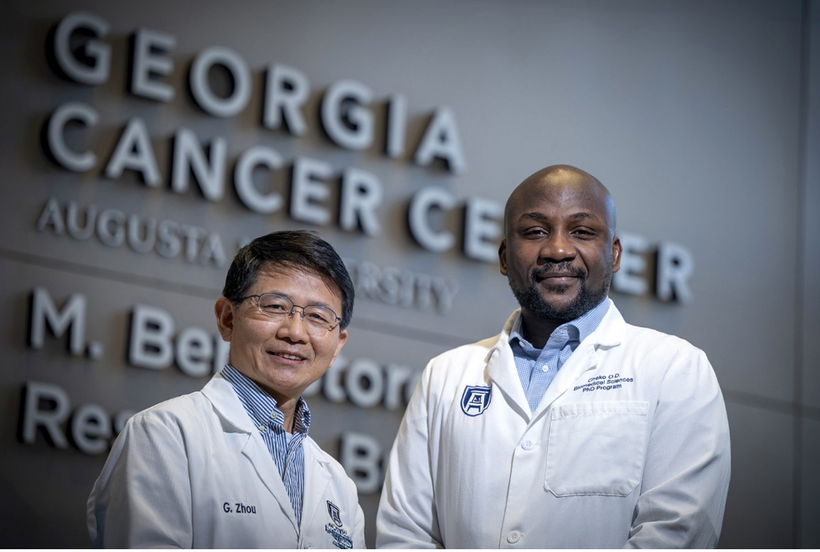
Fueling the Future of Cancer Immunotherapy: Gang Zhou’s Research Takes a Major Step Forward
Cancer immunotherapy has transformed how clinicians approach the treatment of certain blood cancers, but major limitations remain — especially when it comes to sustaining strong, long-lasting immune responses. Gang Zhou, PhD, a leading cancer immunologist at Augusta University’s Georgia Cancer Center and the Immunology Center of Georgia, is tackling these challenges head-on. Zhou’s work focuses on how T cells behave inside the body and how their performance can be enhanced to improve patient outcomes. His lab studies the forces that strengthen or weaken T cell responses, including their functional status, their ability to self-renew and the environmental pressures they face inside tumors. This deep understanding positions him as a key figure in the effort to advance next-generation immunotherapies. Recently, Zhou and his research team were awarded the first Ignite Grant from the Immunology Center of Georgia — a seed program designed to support bold, high-impact translational ideas. Their funded project aims to make CAR-T therapy more effective. CAR-T is a type of immunotherapy in which a patient’s own T cells are genetically modified to recognize and attack cancer cells. While this approach has revolutionized the treatment of certain blood cancers, it still faces obstacles such as limited cell persistence and reduced strength over time. “Our ultimate goal is to engineer T cells that not only survive longer but also remain highly functional, giving patients more durable protection against their disease.” Zhou’s team is addressing this issue by studying how a modified form of STAT5, a transcription factor that plays a key role in T cell survival and function, may help engineered T cells last longer and perform better. The ultimate goal is to create CAR-T therapies that maintain potency, withstand the harsh tumor microenvironment, and offer durable results for patients. The Ignite Grant recognizes not only the promise of this specific project, but also Zhou’s broader expertise in understanding how T cells can be guided, supported, and strengthened to fight cancer more effectively. His research contributes to a growing wave of scientific innovation aimed at improving immunotherapy outcomes for patients with both blood cancers and, potentially, solid tumors — an area where current treatments face significant barriers. As immunotherapy continues to evolve, the work led by Gang Zhou stands as a compelling example of how foundational science, translational research, and clinical ambition can work together to push the field forward. To connect with Dr. Gang Zhou - simply contact AU's External Communications Team mediarelations@augusta.edu to arrange an interview today.