Experts Matter. Find Yours.
Connect for media, speaking, professional opportunities & more.

Modernizing rural health – what it could mean for America
For Americans living outside of cities and in rural and sometimes remote areas of the country, the concept of readily accessible health care just isn’t a reality. However, the idea of expanding broadband internet into rural communities to improve access is one that shares support from all sides of the political spectrum. Just last week, an expert from Augusta University was called up to speak before lawmakers in Congress on the need for this technology and who it could best serve. "Broadband is the gateway to rural schools, businesses and health care providers," said Rep. Angie Craig, a Democrat from Minnesota. Lawmakers raised concerns about the dwindling number of hospitals in rural areas and the need to be competitive when recruiting corporations to do business. "Just the ability in rural America for a physician to pull up an X-ray at their home instead of having to drive to the hospital to look at a patient to know if that is something that’s an emergency," said Rep. Austin Scott, a Republican from Georgia. "One of the biggest needs is tele-psychiatry and tele-mental health," said Dr. David Hess of the Medical College of Georgia. - Spectrum News 1 - July 11 It’s an interesting topic and one that is gaining a lot of attention. How many rural Americans are without access to a doctor or hospital in the country? How much money could be saved by expanding online health care? Online is a viable solution, but are there drawbacks or concerns for patients? And how could expanding broadband and digital health care support issues like mental and maternal health across rural America? If you are a reporter covering this topic – that’s where our experts can help. Dr. David Hess is dean of the Medical College of Georgia and executive vice president for Medical Affairs and Integration at Augusta University. He also helped develop the REACH telestroke network in rural Georgia that now includes about 30 hospitals. Dr. Hess is available to speak with media regarding this topic – simply click on his icon to arrange an interview.

Georgia Southern researchers find adverse childhood experiences associated with short sleep duration
Georgia Southern University professors from the Jiann-Ping Hsu College of Public Health (JPHCOPH) recently completed a study that shows adverse childhood experiences are associated with short sleep duration in adults. Recently, the study was published in SLEEP, the benchmark international journal for sleep and circadian science. The JPHCOPH team looked at nationally representative data from 22,403 adults. Participants in the study who had adverse childhood experiences were more likely to have short sleep duration (less than 6 hours per night) than those without such experiences. Each adverse experience increased the likelihood of insufficient sleep by over 20%, and the association remained throughout adulthood. The study participants were part of the 2011 Behavioral Risk Factor Surveillance System, conducted by the Centers for Disease Control, in which they completed questionnaires detailing childhood experiences of abuse, neglect and household challenges as well as how many hours they sleep nightly as adults. Short sleep duration was not accounted for by mental health challenges or poor physical health, which suggests there are different underlying causes. Over 60% of adults in the U.S. report having experienced at least one adverse childhood experience. The results emphasize the importance of childhood neurodevelopment on long-term health outcomes. Also, the data provides new information on how long adverse childhood experiences may affect sleep and calls for further investigation of the role of childhood experiences in people with sleep challenges. Do you need to know more? Are you looking at stories or to cover how adverse childhood experiences impact sleep and how the long-term effects can follow that individual into adulthood? Let our experts help. Kelly Sullivan, Ph.D., is an expert in epidemiology and neurological diseases and Haresh Rochani, DrPh, is the director of the Karl Peace Center for Biostatistics in the Jiann-Ping Hsu College of Public Health at Georgia Southern University. Both experts are available to speak to this topic – simply click on either icon to arrange an interview.
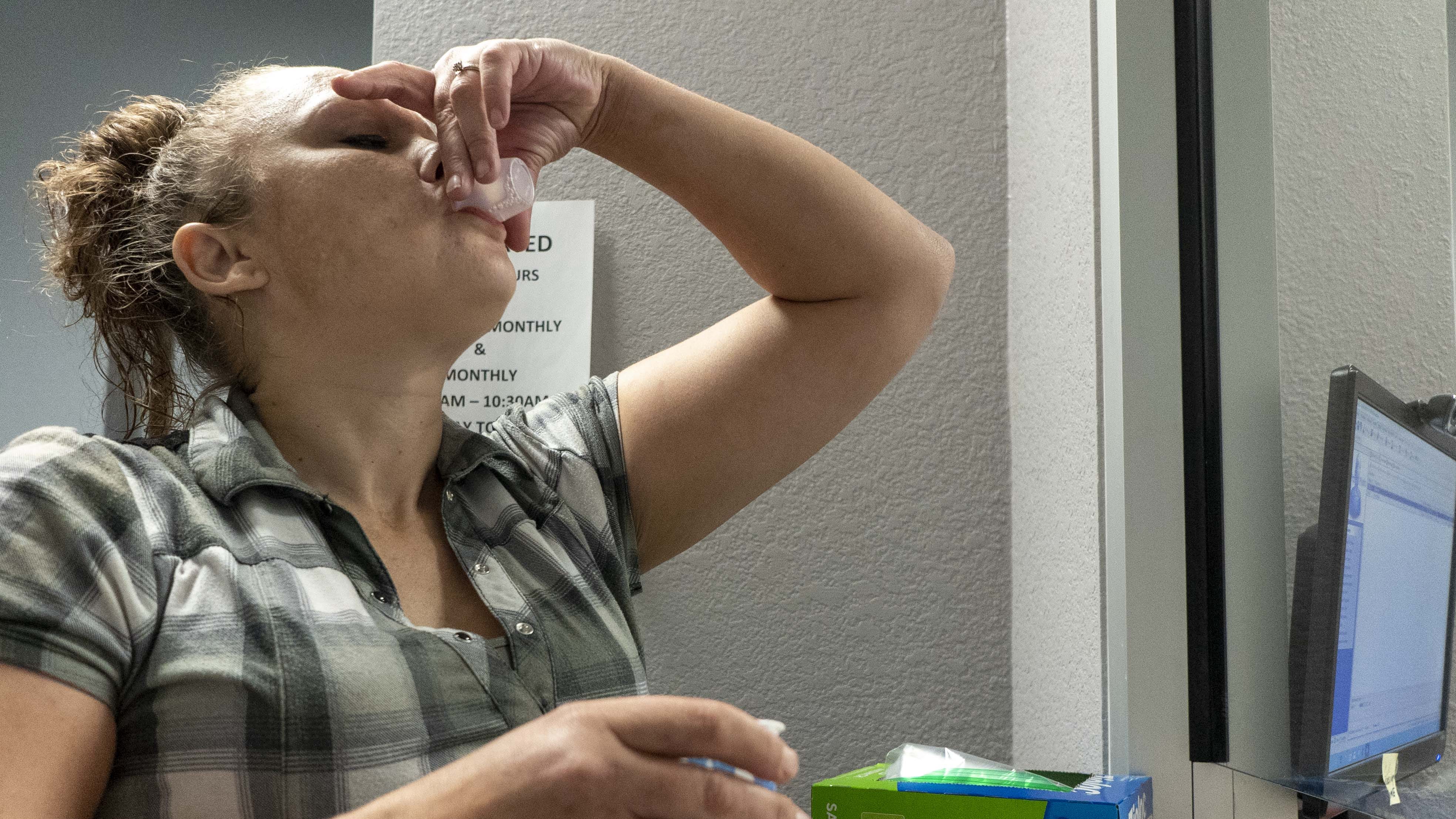
Opioid addiction is gripping America. It’s destroying lives, tearing apart families and devouring resources in policing and healthcare. As medical, mental health and addictions professionals look for solutions, often times accessible and public Opioid Treatment Programs, often known as a Methadone Clinic will open in communities. These clinics bring relief, treatment and support – but they also bring crowds, increased traffic and concern from local residents and the community. These concerns usually find their way to the media, where the attention can quickly turn negative. The solution to avoiding this scrutiny and making sure residents, business owners and community leaders are fully informed about the process, operation and security measures at these clinics are key to their success and integration. Questions such as: How was the site selected? How do you plan to control traffic flow and overcrowding? How will you manage parking and wait times? What are your measures to prevent diversion? Who can I speak to if I have questions or concerns about operations? CARF can speak to best practices, expectations, and requirements for when an opioid treatment program opens. Debbi Witham, Managing Director of Public Policy and is an expert in opioid treatment programs. Debbi is available to speak with media regarding this issue – simply click on her icon to arrange an interview.

It is time for national standards for addiction treatment in America?
America is in the midst of an epidemic, and it is losing. Opioid use often gets the headlines, but substance abuse and addiction is a wider issue with many levels of care and populations The discussion around the country often focuses on causes and criminal justice with less attention paid to the quality and standardization of treatment options and practices. Currently there is no standardized treatment plan in America and it is leaving serious doubts, unfairly, about the effectiveness of treating substance use disorder. “While there are nationally recognized standards for evidence-based care, treatment programs are not required to follow them, and many lack the resources to do so – leaving patients and loved ones with little assurance that a particular program is equipped to deliver high-quality addiction treatment.” Paul H. Earley, MD, DFASAM, MedPageToday.com But what would a standardized addiction treatment system look like? How would it increase transparency and consumer confidence? How would it ensure consistent expectations across the country? What are the costs; can America afford not to implement these strategies? There are a lot of questions and that’s where CARF International can help. Michael Johnson is Managing Director of Behavioral Health at CARF and is an expert in treatment strategies for mental health and substance use disorder. Michael is available to speak with media regarding this topic – simply click on his expert icon to arrange an interview.

Declaring a New Year's Resolution for 2019? Baylor Experts Can Help
WACO, Texas (Dec. 17, 2018) – As 2019 approaches, many Americans are considering ways to improve themselves via New Year’s resolutions. Whether it’s personal, like losing weight or clearing clutter, or it’s professional, such as being a better manager or breaking away from smartphones, the options are wide-ranging. Here is a listing of Baylor University research that might help advise those seeking positive change in the coming year. First and Foremost, Resolve not to Over-resolve Only 10 to 20 percent of people keep their resolutions, says Sara Dolan, Ph.D., associate professor and graduate program director of clinical psychology. She advises setting “bite-sized goals instead of a massive behavior change.” Rather than giving up sugar completely or going all out at the gym, she advises achieving small successes before moving on. Ask Yourself: “Do I really want to work from home?” Many U.S. employees believe working from home – or at least away from the office – can bring freedom and stress-free job satisfaction. A 2018 Baylor University study says, “Not so fast.” The research, led by Sara Perry, Ph.D., assistant professor of management in Baylor University’s Hankamer School of Business, found that: Autonomy is critical to protecting remote employees’ well-being and helping them avoid strain. Employees reporting high levels of autonomy and emotional stability appear to be the most able to thrive in remote-work positions. Employees reporting high levels of job autonomy with lower levels of emotional stability appear to be more susceptible to strain. “Any organization, regardless of the extent to which people work remotely, needs to consider well-being of their employees as they implement more flexible working practices,” the researchers wrote. Read more here. Save Money by being a Better Negotiator In today’s retail climate, where stores struggle to keep up with online competition and customers can compare prices with the ease of their smartphones, the price tag is just a starting point for negotiations, said negotiation expert Emily Hunter, Ph.D., associate professor of management in Baylor’s Hankamer School of Business. “No longer do you need to pay sticker price for everything you buy. The customer is now empowered to have a say in pricing, and even hourly retail workers are often empowered to give price discounts when requested,” Hunter said. Hunter said negotiations – whether in a retail setting or in the workplace – require confidence. “Many people are hesitant to negotiate because they don’t know how or they are worried about the other person’s reaction (Will they think I’m greedy?),” she said. “But practice can increase your confidence in your ability to negotiate. Rejection is less common than you fear, and retail stores especially are often willing to work with you.” She offered the following tips to increase the chances of greater deals at the check-out counter. Resolving to Be More Generous in the New Year Many Americans already have enough “stuff,” and the gift-giving season sometimes adds to that collection of things we really don’t need. Instead of always receiving, how can we resolve to be more generous in the New Year? “Whatever our station, however much money or resources we have, we all have something to share and something to give,” says Andy Hogue, Ph.D., senior lecturer in Baylor’s Honors College who teaches a course on philanthropy and the public good. “I like the idea of thinking in terms of a New Year’s resolution, sort of resolving to be more generous and helping people to think in those ways.” Hogue offers individuals and families four ways to develop a spirit of generosity in the New Year. Home Cooking Saves Money, Encourages Better Diet The more home-prepared foods used, the less risk there is of eating too many calories and fat calories, says Baylor University nutrition expert Janelle Walter, Ph.D., professor of family and consumer sciences and Nutrition Sciences Program coordinator. Home cooking also saves money and allows for more fruits, vegetables and dairy products — which often are missing when pre-prepared products are used — as well as less fat, sugar and salt. Some tips for prepping at home are making a precise list, lining up recipes and lists of ingredients, shopping when you aren’t hungry and preparing five main dishes at a time to see you through a few days. Involve your family in choosing foods, shopping and preparing foods, Walter says. Many simple and quick recipes are on online sites, she said, referencing these from Southern Living. Consider a New Approach to Dieting Meredith David, Ph.D., assistant professor of marketing in Baylor’s Hankamer School of Business, researched successful dieters and how they were different from others. Her research results have received national attention. “Our research shows that instead of creating rules to avoid one’s favorite treats, dieters should focus on eating healthy foods that they enjoy,” David said. “Dieters who restrict themselves from consuming the foods they love most may be setting themselves up for failure. Instead, they may be better off by allowing occasional ‘treats’ and focusing attention on healthy foods that they enjoy and making it a point to include those tasty but healthy foods in their diet.” Read the full article. Be Humble and Helpful In hard times, you know how much a helping hand means — and how humbling those times can be. So it might be good to resolve to look for opportunities to assist in 2019, while remembering not to pat yourself on the back for doing so. A decision to help someone else is influenced by time pressure, number of bystanders, empathy or a person's own distress — but that’s not all, says Baylor researcher Wade Rowatt, Ph.D., professor of psychology and neuroscience. “While several factors influence whether people will volunteer to help, it appears that humble people, on average, are more helpful than individuals who are egotistical or conceited.” Cultivate Patience — and Better Mental Health People who are more patient toward others also tend to be more hopeful, grateful and satisfied with life, says Sara Schnitker, Ph.D., associate professor of psychology and neuroscience. And there is more than one type of patience, including interpersonal patience — dealing with annoying people without losing your cool; handling life hardships — such as illness or unemployment — without frustration or despair; and coping with such daily hassles as traffic jams, computer woes and long lines. In her research, Schnitker invited undergraduates to two weeks of patience training, where they learned to identify feelings and their triggers, regulate their emotions, empathize and meditate. If you want to build your own patience, she recommends following three steps: identify, imagine and sync. First, take a moment to slow down an identify how you are feeling and why you might be feeling that way. Second, try to imagine or reappraise the situation from a different perspective or in a new way that helps you to be calm. Finally, sync with your purpose. Try to connect how what you are doing or enduring helps you pursue larger goals or your life purpose. When Ailing, Talk to A Doctor Instead of Searching the Internet for Answers Rather than heading to the doctor — or even the medicine cabinet — some people turn first to the Internet when they are ailing , according to a Baylor University researcher. Especially for folks who have trouble handling uncertainty, "cyberchondria" — the online counterpart to hypochondria — worsens as they seek answers, says Thomas Fergus, Ph.D., an associate professor of psychology and neuroscience in Baylor's College of Arts & Sciences. “They may become more anxious. And the more they search, the more they consider the possibilities,” he says. Doubts about health also can trigger worries about medical bills, disability and job loss, he said. And that can lead to a Catch-22 of more Googling (sometimes of questionable sources). Rather than giving in to cyberchondria, resolve to call your doctor — and take what you read with a grain of salt. In Conflicts with your Significant Other, Relinquish Power During spats with your spouse or significant other, the most common thing people want is not an apology, but a willingness to relinquish power, says Keith Sanford, Ph.D., professor of psychology and neuroscience in Baylor University's College of Arts & Sciences. That comes in many forms, among them giving a partner more independence, admitting faults, showing respect and being willing to compromise. Following closely behind the desire for shared control was the wish for the partner to show more of an investment in the relationship by such ways as sharing intimate thoughts or feelings, listening and sharing chores and activities, Sanford said. Sleep Better in the New Year Writing a “to-do” list at bedtime may aid in falling asleep, according to a Baylor University study by Michael K. Scullin, Ph.D., director of Baylor’s Sleep Neuroscience and Cognition Laboratory and assistant professor of psychology and neuroscience. Scullin's 2018 research compared sleep patterns of participants who took five minutes to write down upcoming duties versus participants who chronicled completed activities. Scullin suggests that writing a list may allow the brain to “offload” them instead of cycling through them repeatedly. Other hints: Use the bed for sleep rather than studying or entertainment; keep a regular sleep schedule; avoid electronics near bedtime; don’t take long day naps; and stay away from stimulants at least six hours before bedtime. Clear Out Clutter Without Getting Frazzled “Don’t try to organize the entire house in one weekend,” said Elise King, assistant professor in the department of family and consumer sciences. “You are much more likely to complete a task, especially one that you’ve probably been avoiding, if you break it into small goals. Don’t try to clean out an entire room over a weekend; instead, focus on the desk one week, the closet the next, and so forth.” Finally, involve your family, strive to make organization a routine — and reward yourself for your efforts. Break Away from the Smartphone Baylor marketing researchers James Roberts and Meredith David, Ph.D. have conducted numerous studies on the effects of smartphone technology on relationships. Their studies on “phubbing” – phone snubbing – have garnered national and international interest, given the pervasiveness of smartphone technology and its impact on relationships. Their studies have found: Bosses Who “Phone Snub” Their Employees Risk Losing Trust and Engagement “Phubbing” can damage romantic relationships and lead to higher levels of depression People who are phone snubbed by others are, themselves, often turning to their smartphones and social media to find acceptance “Although the stated purpose of technology like smartphones is to help us connect with others, in this particular instance, it does not,” David said. “Ironically, the very technology that was designed to bring humans closer together has isolated us from these very same people.”

Study: Discuss Religion, Spirituality When Treating Young Adults with Severe Mental Illness
Baylor researcher and expert says it’s “critical” that mental health providers be equipped to assess clients’ religion/spirituality A majority of young adults with severe mental illness – bipolar disorder, schizophrenia or major depression – consider religion and spirituality relevant to their mental health, according to a new study from Baylor University’s Diana R. Garland School of Social Work. Holly Oxhandler, Ph.D., associate dean for research and faculty development in the Garland School of Social Work, served as lead author on the study, which was published in the journal Spirituality in Clinical Practice. Researchers examined data from 55 young adults (ages 18-25) with serious mental illness who had used crisis emergency services. Of the 55 young adults interviewed, 34 “mentioned religion or spirituality in the context of talking about their mental health symptoms and service use with little-to-no prompting,” researchers wrote. The sample for the study was racially diverse and gender-balanced. Not all of those interviewed considered themselves religious, as 41 percent answered “other,” “I don’t know” or “none” when asked their religious preference. However, researchers found that religion and spirituality emerged as a unique way in which this sample was able to make sense of their difficult life situations and mental health struggles. “Not only did these young adults struggle with serious mental illness, but they had also experienced extreme adversity – including abuse, poverty, homelessness, addiction, near-death experiences, loss and an overwhelming lack of access to medical and mental health services,” researchers wrote. “Yet, many attempted to explain, make sense of or organize their circumstances through their religious/spiritual perspective and talked about God as a source of comfort and support.” The young adults expressed both positive and negative views of God, prayer and support from religious and spiritual communities. Regardless of their views, the important thing to note, Oxhandler explained, is that they’re talking about these topics – something social workers and counselors traditionally are not often equipped or trained to assess or discuss. “It’s the elephant in the room,” Oxhandler said of discussions of religion and spirituality. “If we continue to ignore it, we’re ignoring a huge component of peoples’ lives that may be tied to the clinical issue.” Oxhandler, who has researched this area extensively, said such discussions can help drive subsequent treatment options. “As mental health care providers discern what mental health services to provide or coping strategies to recommend, it’s especially important they understand the role of religion/spirituality in the lives of the vulnerable young adults they serve,” she said. Researchers also found that those surveyed described using positive religious coping, negative religious coping or experiences, discussed their relationship with God/Higher Power and unpacked the role of their support systems and faith. Positive religious coping included prayer, reading religious texts, support from their religious and spiritual communities and identifying religious and spiritual meaning in difficult situations. Negative religious coping or experiences included having a negative experience with a religious organization not being supportive or receiving hurtful messages from the religious community. “Those who discussed their relationship with God or a higher power discussed God providing a sense of comfort or protection, accepting them for who they are or positively intervening in their lives,” Oxhandler said. “Among those who unpacked the role of their support systems and faith, they often described family and friends referencing religion or God for support, and some even offered recommendations for others struggling with mental illness that involve religion and spirituality.” Some of those interviewed shared that they found the mention of God or religion by family and friends less than helpful. For example, a 22-year-old white female with no religious identification mentioned in her interview that a family member “tries to tell me that going to church will be better for me because it will help me find peace, and it really does quite the opposite.” Interestingly, researchers noted that nearly all participants who reported negative experiences with religion and spirituality also reported utilizing positive religious and spiritual coping or having a positive relationship with God. Oxhandler said such complexity highlights the importance of including religion and spirituality during the initial assessment with a client. “It’s critical that mental health care providers be well equipped and trained to assess for the complex role of religion and spirituality in the lives of young adults with serious mental illness, recognizing that it could appear to be a tremendous source of support and resilience and/or a source of pain and discomfort, if even a part of their lives at all,” she said. ABOUT THE STUDY “Religion and Spirituality Among Young Adults With Severe Mental Illness,” published in the journal Spirituality in Clinical Practice, is authored by Holly K. Oxhandler, Ph.D., L.M.S.W., assistant professor and associate dean for research and faculty development, Diana R. Garland School of Social Work, Baylor University; Sarah C. Narendorf, Ph.D., L.C.S.W., assistant professor, Graduate College of Social Work, University of Houston; and Kelsey M. Moffatt, M.S.W., Diana R. Garland School of Social Work, Baylor University. ABOUT BAYLOR UNIVERSITY Baylor University is a private Christian University and a nationally ranked research institution. The University provides a vibrant campus community for more than 17,000 students by blending interdisciplinary research with an international reputation for educational excellence and a faculty commitment to teaching and scholarship. Chartered in 1845 by the Republic of Texas through the efforts of Baptist pioneers, Baylor is the oldest continually operating University in Texas. Located in Waco, Baylor welcomes students from all 50 states and more than 80 countries to study a broad range of degrees among its 12 nationally recognized academic divisions. ABOUT DIANA R. GARLAND SCHOOL OF SOCIAL WORK Baylor University’s Diana R. Garland School of Social Work is home to one of the leading graduate social work programs in the nation with a research agenda focused on the integration of faith and practice. Upholding its mission of preparing social workers in a Christian context for worldwide service and leadership, the School offers a baccalaureate degree (B.S.W.), a Master of Social Work (M.S.W.) degree and three joint-degree options, M.S.W./M.B.A., M.S.W./M.Div. and M.S.W./M.T.S., through a partnership with Baylor’s Hankamer School of Business and George W. Truett Theological Seminary, and a Ph.D. program. Visit www.baylor.edu/social_work to learn more.

‘The surprise, and the up side, is that episodic memories from before the children’s treatment were spared,’ Baylor researcher says Children with certain types of brain tumors who undergo radiation treatment are less likely to recall the specifics of events they experienced after radiation than to remember pre-treatment happenings, according to a Baylor University study comparing them to children with healthy brains. The finding is significant because children after treatment had less volume in the hippocampus — a part of the brain that plays an important role in memory. But while such a decrease usually is associated Alzheimer’s disease, dementia, brain injury, epileptic amnesia, encephalitis and aging, with those conditions both remote and recent memories are impaired, said lead author Melanie Sekeres, Ph.D., director of Sekeres Memory Laboratory at Baylor University. “The surprise, and the up side, is that episodic memories from before the children’s treatment were spared,” Sekeres said. For the study, published in The Journal of Neuroscience, researchers focused on “autobiographical memory,” which is linked to unique personal events and involves the recollection of emotional and perceptual details that allow a person to mentally re-experience the event, said Sekeres, assistant professor of psychology and neuroscience in Baylor’s College of Arts & Sciences. Radiotherapy and chemotherapy are used to treat the most common malignant brain tumor in children — a medulloblastoma. The reduced volume of the hippocampus is likely associated with radiation’s impact on the development of new cells in the nervous system, including the growth of new neurons in the hippocampus, or neurogenesis. “We know that these new cells play crucial roles in regulating memory and spatial learning, which is required to navigate. These treatments limit the brain’s ability to produce these new cells, which, in turn, limits the ability to form new memories,” Sekeres said. Research participants were 13 child survivors of brain tumors who had previously received radiotherapy and chemotherapy treatment at least one year before the study. Twenty-eight healthy youths of similar ages (ranging from 7 to 18) also were recruited for the study, conducted with The Hospital for Sick Children in Toronto, Ontario, Canada. All the youths completed the Children’s Autobiographical Interview — a standardized memory test — and underwent magnetic resonance imaging (MRI) of the brain. In individual interviews, children in both groups also were asked to recall memories from personal events that occurred at a specific time and place. Children were asked to recall a very old memory from an event before their radiation treatment (or an equally old memory for the healthy children) and a recent memory from within the past month. They were offered a list of events such as a birthday party, family trip, graduation and getting a pet but were told that they could choose another happening. The interview allowed children to freely recall without prompting before being asked general and specific questions about the event. “They have a hard time forming new, detailed memories,” Sekeres said. For example, when talking about a recent birthday party for a friend, they might tell how they met the friend and what that individual likes to do, but few specifics such as what they wore, the type of cake, what friends were there and what activities they did at the party, she said. “Such specific details might seem trivial, but these are precisely the kinds of details that allow us to vividly replay important events in our lives,” Sekeres said. “For most events, though, even healthy people forget a lot of specific details over time because we typically don’t need to retain all that incidental information. Some forgetting is normal and adaptive, and what we remember is the gist of an older event.” The patients were just as capable as healthy children of recalling these older memories, she said. But for children with brain tumors who have undergone radiation, the study suggested “deficits in their ability to either encode and/or retrieve highly detailed memories for personal events,” Sekeres said. “And those are the kind of memories that allow us to understand who we are and give us rich personal lives. “The study identifies an area of cognition that is inadvertently impacted by standard treatment, which has real consequences for the quality of life of the survivors. The physicians’ ultimate goal is to allow their patients to survive and to live as well as possible,” Sekeres said. “Although these treatments are often crucial in the effective management of the cancer, if the physicians and the family know there are these unintended side effects, that may be an additional factor to consider when exploring the treatment options.” ABOUT THE STUDY The study — “Impaired recent, but preserved remote, autobiographical memory in pediatric brain tumor patients” — was conducted with the Brain Tumor Program and the Program in Neurosciences and Mental Health at The Hospital for Sick Children in Toronto, Ontario, Canada. Funding was provided through the Canadian Institutes of Health Research. ABOUT BAYLOR UNIVERSITY Baylor University is a private Christian University and a nationally ranked research institution. The University provides a vibrant campus community for more than 17,000 students by blending interdisciplinary research with an international reputation for educational excellence and a faculty commitment to teaching and scholarship. Chartered in 1845 by the Republic of Texas through the efforts of Baptist pioneers, Baylor is the oldest continually operating University in Texas. Located in Waco, Baylor welcomes students from all 50 states and more than 80 countries to study a broad range of degrees among its 12 nationally recognized academic divisions. ABOUT BAYLOR COLLEGE OF ARTS & SCIENCES The College of Arts & Sciences is Baylor University’s oldest and largest academic division, consisting of 25 academic departments and seven academic centers and institutes. The more than 5,000 courses taught in the College span topics from art and theatre to religion, philosophy, sociology and the natural sciences. Faculty conduct research around the world, and research on the undergraduate and graduate level is prevalent throughout all disciplines. Visit College of Arts & Sciences.

Can Hollywood help lift the stigma on mental health?
When A Star is Born was released to theatres – it had high expectations. It was a hit at international film festivals and Oscar buzz was already starting. Loaded with stars from stage, screen, and the music industry, it was guaranteed to bring in the audiences and pack theatres. While critics are raving about the performances, the message the film is bringing is also resonating with audiences as well. The story deals with characters attempting to overcome addictions as well as suicide. It’s a film that has people talking about serious issues. But is it Hollywood’s job to educate people about issues such as mental health? With the lines between education and entertainment blurring – is this a platform that could serve the wrong purposes? And with all things celebrity, is there a risk to glorifying acts of suicide or addiction? There are a lot of questions and that’s where the experts from CARF International can help. Michael Johnson is Managing Director of Behavioral Health at CARF and is an expert in mental health and substance use disorder. Mike is available to speak with media regarding this topic – simply click on his icon to arrange an interview.

Women often don't label their sexual assaults as rape. Our experts can explain.
Many sexual violence survivors do not label their experiences as rape but instead use more benign labels, such as “bad sex” or “miscommunication.” Laura C. Wilson, an assistant professor of psychology at the University of Mary Washington, led a review of 28 academic studies to estimate how often women who’ve been sexually assaulted do not label their experience as rape. Across the studies, the researchers find that 60.4 percent of women, on average, did not recognize their experience as rape even though it fit the definition — an unwanted sexual experience obtained through force or the threat of force or a sexual experience they did not consent to because they were incapacitated. “This finding has important implications because it suggests that our awareness of the scope of the problem may underestimate its true occurrence rate, depending on the type of measurement,” the authors write. “This impacts policy reform, allocations of mental health services, survivors’ perceptions of their experiences, and society’s attitudes toward survivors.” For more information on this study, visit: http://journals.sagepub.com/doi/abs/10.1177/1524838015576391 Laura C. Wilson is available to speak with media regarding this topic and study. To contact her, simply click on her icon to arrange an interview.

Community is key for those recovering from a mass shooting
The man accused of killing 17 people and injuring 14 more at Marjory Stoneman Douglas High School in February is set to appear in court Wednesday. Meanwhile, survivors of the mass shooting are still grappling with the aftermath of that day. Laura Wilson, co-author and editor of "The Wiley Handbook of the Psychology of Mass Shootings" and an assistant professor of psychology at the University of Mary Washington in Fredericksburg, recently talked about that struggle in an American Psychological Association article. "Simply by definition, mass shootings are more likely to trigger difficulties with beliefs that most of us have, including that we live in a just world and that if we make good decisions, we'll be safe," she is quoted as saying. According to the article: "The National Center for PTSD estimates that 28 percent of people who have witnessed a mass shooting develop post-traumatic stress disorder (PTSD) and about a third develop acute stress disorder. "Research also suggests that mass shooting survivors may be at greater risk for mental health difficulties compared with people who experience other types of trauma, such as natural disasters. A study led by former Northern Illinois University (NIU) graduate student Lynsey Miron, PhD, after the 2008 shootings on NIU's campus, found that although a large percentage of mass shooting survivors were either resilient or displayed only short-term stress reactions, about 12 percent reported persistent PTSD, a number that's higher than the average prevalence of PTSD among trauma survivors as a whole (Behavior Therapy, Vol. 45, No. 6, 2014). "What's critical, psychologists' research suggests, is to ensure that victims feel connected to their communities in the aftermath of mass violence and that they have ongoing support available to them." Dr. Wilson is available to speak with media regarding this subject. Simply click on her icon to arrange an interview. Source:





