Experts Matter. Find Yours.
Connect for media, speaking, professional opportunities & more.

Professor Sangeeta Khorana made a Fellow of the Academy of Social Sciences
Professor Sangeeta Khorana, professor of international trade policy at Aston University, has been made a Fellow of the Academy of Social Sciences Fellows are elected for their contributions to social science, including in economic development, human rights and welfare reform The 2025 cohort of 63 Fellows will join a 1,700-strong Fellowship with members from academia, the public, private and third sectors. Professor Sangeeta Khorana, professor of international trade policy at Aston University, has been made a Fellow of the Academy of Social Sciences as part of the Autumn 2025 cohort. The 63 new Fellows have been elected from 39 UK organisations, comprising 29 higher education institutions, as well as think tanks, non-profits, business, and from countries beyond the UK including Australia and China. The Academy of Social Science’s Fellowship comprises 1,700 leading social scientists from academia, the public, private and third sectors. Selection is through an independent peer review which recognises their excellence and impact. Professor Khorana has more than 25 years of academic, government and management consulting experience in international trade. She has worked for the Indian government as a civil servant and on secondment to the UK Department for Business and Trade. Her expertise includes free trade agreement (FTA) negotiations and World Trade Organization (WTO) issues. As well as sitting on various expert committees, Professor Khorana is an advisor on gender and trade to the Commonwealth Businesswomen’s Network in London and serves on Foreign Investment Committee of the PHD Chambers of Commerce and Industry, India. The Autumn 2025 cohort of Fellows have expertise in a range of areas including educational inequalities, place-based economic development, human rights protection, the regulation of new technologies, and welfare reform, highlighting the importance, breadth and relevance of the social sciences to tackling the varied challenges facing society today. As well as excellence in research and professional applications of social science, the new Fellows have also made significant contributions beyond the academy, including to industry, policy and higher education. Professor Khorana said: “I am deeply honoured to be elected a Fellow of the Academy of Social Sciences. This recognition underscores not only the importance of international trade policy as a driver of inclusive and sustainable growth, but also the role of social sciences in shaping fairer and more resilient societies. At Aston University, my research seeks to bridge academia, government and industry to inform evidence-based trade policy for global cooperation. I am proud to contribute to the Academy’s mission of demonstrating how social science knowledge and practice can address some of the most pressing challenges of our time.” President of the Academy, Will Hutton FAcSS, said: “It’s a pleasure to welcome these 63 leading social scientists to the Academy’s Fellowship. Their research and practical applications have made substantial contributions to social science and wider society in a range of areas from international trade policy and inclusive planning systems through to innovative entrepreneurship and governing digital technologies. We look forward to working with them to promote further the vital role the social sciences play in all areas of our lives.”

Before you scroll past thinking, “Oh, another scam alert,” please pause. This isn’t your average “don’t answer spam calls” notice. What follows is an examination of the growing sophistication of grandparent scams—complete with call centers, scripts, and even AI voice cloning. More importantly, it’s about how to protect yourself and, especially, the older members of your family. Read on—not just for awareness, but for fundamental tools to keep your loved ones safe. Even Elvis Isn't Safe From Scammers You know the world has gone topsy-turvy when even the King of Rock 'n' Roll isn't immune to fraud. I've written before about the recent attempt to scam Elvis Presley's Graceland estate, but a recent story about senior fraud really got my blood boiling. U.S. authorities in Boston just charged 13 people connected to what I can only describe as a "grandparent scam industrial complex" – a sophisticated operation that bilked over 400 elderly Americans out of more than $5 million. These weren't your run-of-the-mill phone scammers calling from their basement. Oh no. These criminals were running call centers with scripts, managers, and daily money-making leaderboards like they were selling insurance, not breaking hearts. The math alone should make you furious: $5 million divided by 400 victims equals about $12,500 per person. That's not pocket change – that's someone's emergency fund, their vacation savings, or money they've been carefully setting aside for healthcare costs. The Grandparent Scam: Emotional Manipulation 101 If you're not familiar with grandparent scams, buckle up. These predators have turned family love into their business model, and they're disgustingly good at it. Here's their playbook: Step 1: The Panic Call – "Grandma, it's me! I'm in jail and need bail money RIGHT NOW!" Step 2: The Identity Theft – Using social media details (yes, those cute Facebook posts about little Johnny's soccer game), they sound convincingly like your grandchild. Some are even using AI voice-cloning technology. Step 3: The Time Crunch – Everything's an emergency. No time to think, no time to verify. Just panic and send money. Real emergencies, by the way, allow time for a phone call to confirm details. Step 4: The Collection – Cash via courier, rideshare driver pickup, wire transfers, even Bitcoin. Anything except the legitimate ways actual legal systems collect bail money (spoiler alert: the good guys don't send Uber drivers to your house). The Boston Grandparent Fraud Case: Scamming at Scale The level of organization in this Boston case reads like a twisted business manual. These criminals weren't just winging it – they had: • Dedicated "Opener" staff who made initial contact with victims • Specialized "Closers" who pretended to be lawyers demanding payment • Management training programs for their scam employees • Daily performance systems (because nothing says "organized crime" quite like gamifying elderly financial abuse) A number of things bothered me about this case The fraudsters got over $5 million from 400 victims. The simple math shows that, on average, each victim would have lost $12,500 – that’s not “walking around” money. I suspect many would have had to tap into a variety of savings accounts or possibly borrow from others to source funds on short notice. This creates an extra degree of hardship for victims who are struggling to manage on a fixed income. The average age of the victims was 84. This breaks my heart. The oldest in this cohort are especially vulnerable. At this age, many seniors live alone or are more isolated, making them easier prey for these deceitful tactics. Many of them are still uninformed about how these scams operate. The scammers showed a very high level of sophistication. According to court documents from the U.S. Department of Justice, District of Massachusetts (2025), the scammers operated a sophisticated “call center” with technology at multiple sites, enabling them to place a massive number of calls to unsuspecting victims. • These scams would begin with an “Opener” employee, who would call victims and read a script (see below) pretending to be a grandson or granddaughter who was in an accident. • Then, a “Closer” would allegedly follow up with another call, pretending to be their grandchild’s attorney, asking for a sum of money to pay for their grandchild’s fees due to the accident. Each of these call center locations had managers overseeing staff who trained, supervised, and paid employees. The most sickening part? They kept detailed records of how much money they stole each day, treating vulnerable seniors like ATM machines with feelings. Here is an actual photo of their “Leaderboard” taken as evidence in the Boston case. When it came to handling cash, they also had a plan for that. Most often, they used unsuspecting rideshare drivers whom they ordered to do a package pickup at the victim’s house. And these heartless criminals often went back for seconds and thirds. Using lines designed to trigger seniors into emptying their bank accounts. They would say things like "Oh, there's been a mix-up," or "A pregnant woman's baby was lost in the crash" – any lie to squeeze more money from people who'd already been devastated once. Now, I’ve been in enough boardrooms to know that leaderboards usually track sales of widgets, mortgages, or, at worst, how many stale muffins are left in the breakroom. But imagine walking into work and your boss says, “Congratulations, you scammed the most grandmas today—you win Employee of the Month!” That’s not just evil, it’s the kind of thing that should earn you a permanent bunk bed in a tiny jail cell. And using Uber drivers to pick up cash? Please. The only thing Uber should be picking up is takeout and slightly tipsy people at 11 p.m.—not Grandma’s retirement savings. Some of These Scams Are Coming From Inside Canada Here's where this story hits close to home. While we might imagine these scams operating from some far-off location, some of the biggest operations have been running right here in Canada. In March 2025, Montreal police arrested 23 people connected to a massive network that allegedly defrauded seniors across 40 U.S. states of $30 million over three years. The suspected ringleader, Montreal developer Gareth West, allegedly ran call centers from Quebec properties and laundered the proceeds into luxury real estate. West remains at large, proving that sometimes the worst criminals are hiding in plain sight in Canadian suburbs. The Canadian Reality Check According to the Canadian Anti-Fraud Centre, emergency or 'grandparent scams' have become one of the fastest-growing crimes targeting seniors in Canada, with reported losses rising from $2.4 million in 2021 to over $11.3 million in 2023. Here's where it gets even more interesting. Those figures are just the losses for gradparent fraud that are reported – experts estimate the true losses are at least ten times higher since only 5-10% of fraud victims come forward. Let that sink in: we could be looking at over $100 million in actual losses annually in Canada alone. Here’s the part that really stings: no one is exempt. Not me, not you, not even that friend who insists they “don’t answer unknown numbers.” (Sure, Jan. We all know you still pick up when it says “potential spam.”) This isn’t just about losing money—it’s about losing confidence. The shame, the self-doubt, and the “How could I fall for that?” spiral are often worse than the financial loss. I’ve seen strong, capable people withdraw after being scammed, too embarrassed to tell their own families. And honestly—I get the same chill when I read these stories: Would I have caught it in time? It’s a reminder that vigilance is like flossing—we all know we should do it daily, and yet… sometimes we forget until it hurts. Supporting an Elder Who’s Been Scammed Here’s where we need to step up as families and communities Practical Support: • Help them file a report with the police and the Canadian Anti-Fraud Centre. • Contact their bank to determine if the funds can be recovered. • Lock down social media and adjust privacy settings so future scammers have less ammunition. Emotional Support: • Listen without judgment. Don’t say, “I would never have fallen for that.” (Trust me—you might.) or “you know better, Granddad”. • Normalize the experience: this can happen to anyone. If AI can clone voices and manipulate emotions, it’s not about intelligence—it’s about being human. • Follow up regularly. Shame makes people pull back, so check in to ensure they’re not withdrawing or losing confidence. Your Family’s Fraud Fighting Toolkit Look, I've spent over 30 years in the financial industry, and I can tell you that preventing fraud is always easier than recovering from it. Here's your family's defence strategy: The P-A-U-S-E Method Pause – Don't act immediately, no matter how urgent the request sounds. Ask questions only family members would immediately know ("What's Mom's maiden name?") Use known phone numbers to call your grandchild directly and verify information Set up systems to protect family members (like a secret family password) Explain to others – share this information widely with all family members Know the Red Flags • Demands for immediate action (real emergencies allow verification time) • Requests for secrecy ("Don't tell Mom and Dad!") • Payment via courier, rideshare, wire transfer, or cryptocurrency • Emotional manipulation ("I'm so scared, Grandma!") • Any request for cash payment to resolve legal issues Family Password System Set up a secret word or phrase that only your family knows. Make it something memorable but not guessable from social media. "Fluffy" (your childhood dog) is better than a pet name you posted on a recent social media post. What to Do If You're Targeted Stop. Don't. Send. Money. Instead: • Hang up immediately • Call your local police to file a report • Report to the Canadian Anti-Fraud Centre: 1-888-495-8501 or visit antifraudcentre-centreantifraude.ca • If you've already sent money, contact your bank immediately • Tell other family members what happened – you're not the only target These criminals exploit the most powerful human emotions: love, fear, and the desire to protect our families. They've turned grandparents' natural instinct to help their grandchildren into a multi-million-dollar crime operation. But here's what they're banking on (pun intended): that we'll be too embarrassed to talk about it, too confused to verify it, and too panicked to think clearly. Don't give them that satisfaction. Remember, the average age of victims in the Boston case was 84. These aren't people who have time to recover from financial mistakes. Every dollar stolen from a senior is a dollar that won't be there for healthcare, housing, or basic dignity in their final years. We Can Fight Back Knowledge is power, and conversation offers protection. The more we discuss these scams openly – around dinner tables, in community centres, at family gatherings – the more we hinder these criminals from succeeding. Share this post with the seniors in your life. Not because they're naive, but because they're caring. And because caring people deserve to know how heartless criminals are trying to exploit their love. What is your family doing to protect against fraud? What are your strategies and ideas for keeping our loved ones safe? I’m also particularly interested in what financial institutions and various government agencies are doing these days to combat fraud and protect this vulnerable group. As I research this topic more, I’d love to hear from you. Remember: Real grandchildren in genuine emergencies can wait five minutes for you to confirm who you're talking to. Scammers can't. Helpful Resources: • Canadian Anti-Fraud Centre: 1-888-495-8501 • Report online: antifraudcentre-centreantifraude.ca • For more retirement security tips, visit retirewithequity.ca Stay safe. Don't Retire - Rewire! Sue

ChristianaCare Hospital, West Grove to Open Mid-August 2025
ChristianaCare is opening its first neighborhood hospital in the company’s 188 year history — ChristianaCare Hospital, West Grove. Set to open in mid-August, this facility offers a new model of emergency and acute care right in the heart of southern Chester County. The exact opening date will be confirmed following final inspection by the Pennsylvania Department of Health, which is scheduled to occur in the first week of August. A Modern Hospital, Right in the Neighborhood Located at 1015 West Baltimore Pike, the 20,000-square-foot hospital will operate 24/7, offering around-the-clock care in a modern, easy-to-access setting. Developed in partnership with Emerus Holdings, Inc., the nation’s leading developer of neighborhood hospitals, this facility brings high-quality acute and emergency care directly into the community. It will be staffed with board-certified emergency physicians, skilled nurses and clinical specialists, all dedicated to delivering patient-first, efficient and compassionate care. “It’s an honor and privilege to expand access to high-quality care for our neighbors in southern Chester County,” said Janice Nevin, M.D., MPH, president and CEO of ChristianaCare. “We will be opening our doors for the families in this community with a steadfast commitment to being their trusted health care partner. We’re grateful for the opportunity to bring love and excellence to those we will serve.” Convenient, Comprehensive Services ChristianaCare Hospital, West Grove is designed to meet a wide range of everyday medical needs. Key features include: A full-service emergency department with 10 treatment rooms. A 10-bed inpatient unit for overnight stays, observation and diagnostics. Advanced imaging and lab services, including ultrasound, CT scan and X-ray. Virtual access to specialists in such areas as cardiology, critical care and infectious disease. The emergency department is equipped to treat conditions such as falls, injuries, heart attacks and strokes. Patients requiring surgery or more complex care will be stabilized and seamlessly transferred to a hospital with more expanded service offerings based on the clinical needs of the patient. “This neighborhood hospital brings the right mix of services to support the health and well-being of our neighbors,” said Pauline Corso, president of ambulatory network continuity and growth at ChristianaCare. “We’re excited to bring care close to home to meet the needs of the community. We’re here to stay and grow alongside this community.” The project has received strong local support and was made possible in part by generous grants from the Commonwealth of Pennsylvania and the Chester County Board of Commissioners — Josh Maxwell, Marian Moskowitz, and Eric Roe — whose leadership helped bring this vision to life. Health Center Expands Access to Primary and Specialty Care As part of its long-term investment in the West Grove Campus, ChristianaCare has also purchased the building at 900 W. Baltimore Pike, across the street from the hospital. This facility currently houses a ChristianaCare primary care practice and imaging services, offering walk-in X-rays and scheduled mammography and ultrasound appointments. This health center will continue to evolve to meet the growing needs of the community. Meeting Regional Needs with a Broader Vision ChristianaCare is expanding its neighborhood hospital model to address care gaps across southeastern Pennsylvania. New hospitals are being planned for Aston and Springfield Townships in Delaware County, with the Aston location already under construction and expected to open in late 2026. In addition, ChristianaCare was the successful bidder for Crozer Health outpatient centers in Glen Mills, Havertown, Broomall and Media, further strengthening its regional footprint and ability to deliver timely, high-quality care. A Legacy of Care in Southeastern Pennsylvania ChristianaCare’s presence in the region is long-standing. The organization currently provides primary care at three Chester County locations — Kennett Square, Jennersville and West Grove — and recently opened a cardiology practice in West Grove. In neighboring Delaware County, the Concord Health Center in Chadds Ford offers a wide range of services, including primary care, women’s health, sports medicine, and behavioral health. Together, these sites serve as the medical home for more than 25,000 residents, underscoring ChristianaCare’s deep commitment to delivering accessible, high-quality care where it’s needed most.

Strategies for Minimizing Rising Risks to Mobile Apps from Privacy Laws
As mobile apps become more central to customer engagement, they’re also drawing closer scrutiny under global data privacy laws. In this expert-backed article, Antonio Rega, Managing Director at J.S. Held, and Ian Cohen, CEO of LOKKER, outline how businesses can identify hidden privacy risks—particularly those created by third-party SDKs and what steps they can take to stay compliant. What’s covered: • How data minimization and purpose limitation apply to mobile architecture • Real-time consent dilemmas and SDK-related exposure • Transparency gaps in mobile data flows • Upcoming enforcement trends and what they signal for app owners With decades of combined experience in digital forensics, risk, and data governance, Rega and Cohen bring sharp insight into a fast-evolving regulatory landscape. Whether you’re developing, auditing, or overseeing mobile platforms, this article breaks down what’s at stake and how to protect both users and your organization. Looking to connect with Antonio Rega? Click on his profile icon to arrange an interview or get deeper insights into data privacy, risk, and mobile app compliance. For any other media inquiries, contact : Kristi L. Stathis, J.S. Held +1 786 833 4864 Kristi.Stathis@JSHeld.com.
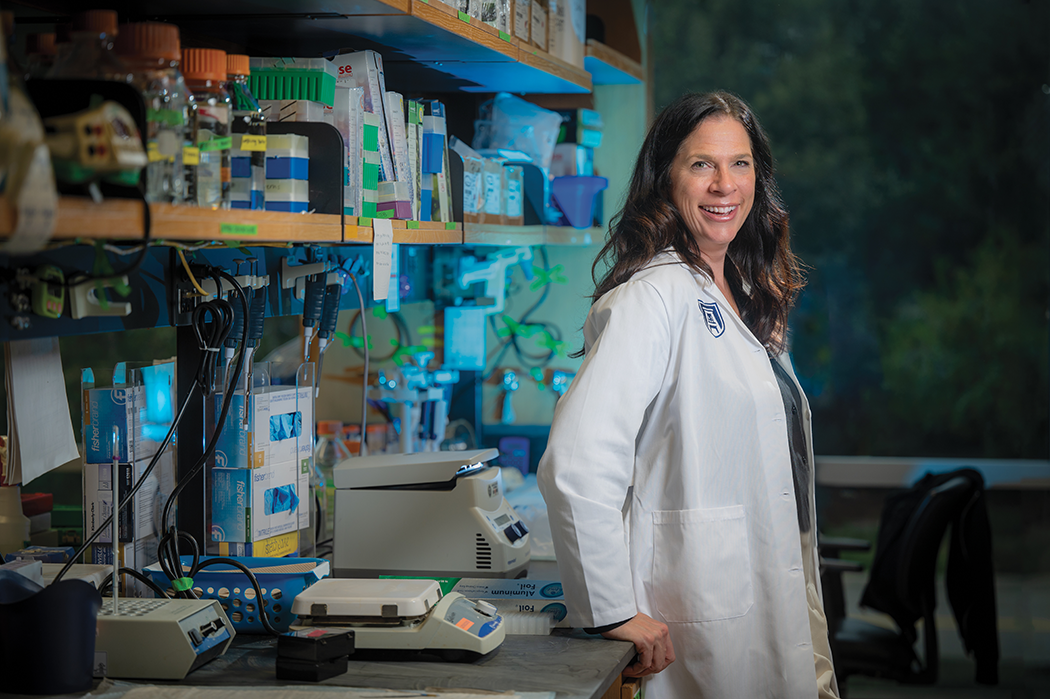
Augusta University named NIH Specialized Center of Research Excellence on Sex Differences
Jennifer C. Sullivan, PhD, dean of The Graduate School at Augusta University, has dedicated her research to better understand why blood pressure increases in hypertension and raising awareness to the dangers of not paying attention to heart health, particularly among women. Throughout her career, Sullivan has been continuously funded by the National Institutes of Health (NIH) and the American Heart Association since becoming a tenure-track faculty member in 2008, and now she has a chance to take her research further after securing a five-year, $7.5 million grant to have Augusta University designated as a Specialized Center of Research Excellence on Sex Differences (SCORE) by the NIH’s Office of Research on Women’s Health. It’s a distinction that places AU among 10 other leaders in research for the field, including Brigham and Women’s Hospital, Cedars-Sinai Medical Center, Emory University, Johns Hopkins University, Massachusetts General Hospital and Harvard Medical School, the Mayo Clinic, the Medical University of South Carolina, the University of Colorado and Yale University. The University of California, Los Angeles has two SCORE programs. “I’m so proud and excited for this opportunity because this has been what I have focused my research program on for my entire career, and to be able to advance it with a program like this, where we can actually build a unique program focused on an area that can make a difference, is just so much fun,” Sullivan said. “Just the fact that Augusta will be included on this list, attached to an organization of the caliber of NIH, will provide opportunities that we’ve never had before, especially for our students and younger researchers.” Sullivan’s SCORE project, “Improving awareness of women with hypertension: ROAR (Rural, Obese, At Risk),” focuses primarily on the fact that, while young women are considered “protected” from hypertension and the associated cardiovascular risk relative to age-matched men, the elimination of hypertension is projected to have a larger impact on cardiovascular disease (CVD) mortality in women. “The group of people with the highest risk of death from hypertension is in the rural South of the U.S., specifically Black women are particularly vulnerable to developing hypertension and CVD,” Sullivan said. According to Sullivan’s research and information available from the American Heart Association (AHA), approximately 19 million deaths were attributed to CVD globally in 2020, an increase of about 20% from 2010. Both Sullivan and the AHA state that cardiovascular disease remains the leading cause of death for both men and women in the United States, and that hypertension is a major modifiable risk factor for CVD. Sullivan said, “It has been suggested that eliminating hypertension would reduce CVD mortality by over 30% in men and 38% in women, but a critical barrier to limiting premature death from CVD is lack of awareness surrounding the risks of CVD. Our overall goal in this new funded project is to transform academic and community understanding of sex as a biological variable in the consideration of hypertension.” The three research projects include Sullivan’s lead project on high fat diets, a project on systemic lupus erythematosus (SLE) disproportionately affects young women led by Erin Taylor, PhD, at the University of Mississippi Medical Center, and another project looking at the role of inflammation and how immune cells are activated in SLE led by Michael Ryan, PhD, at the University of South Carlina’s School of Medicine. But there is more to SCORE than just conducting research. Each SCORE team is also responsible for a career enhancement core and a leadership administrative core. “What really sets these grants apart are the emphasis on the career enhancement and leadership administrative cores. The Career Enhancement Core is designed to be a bit open ended for each SCORE, but in talking to the NIH, what they were most excited about in our project is the community outreach piece we designed. “Our grant includes people across the entire campus, including Augusta University’s Medical College of Georgia, the College of Allied Health Sciences, the College of Education and Human Development and multiple campus partners including some of our sororities on campus and the Center for Writing Excellence,” Sullivan said. “More specifically, the COEHD is able to extend our outreach efforts to our local schools to begin educating children on the importance of screening, and our sororities are obviously connected with other chapters across the southeast which helps us spread our message, as well.” Sullivan notes that, through this portion of the project alone, there will be numerous opportunities to include students from Augusta University’s CAHS, College of Nursing, Department of Kinesiology, the Biomedical Sciences PhD program and the proposed School of Public Health. Marlo Vernon, PhD, associate professor at MCG and researcher for the Georgia Cancer Center, and Amanda Behr, chair of the Medical Illustration Program in CAHS, are also involved in various stages of the project. “The other thing the Career Enhancement Core will do is provide pilot grants to three research projects each year for early-stage investigators. We’ll also be able to fund sabbaticals for graduate students or postdocs to go someplace else and learn cutting edge techniques from other experts, so there is a lot built in that will help us support up-and-coming researchers,” Sullivan said. “We’re now part of this consortium, and they have a once-a-year, in-person meeting at the NIH offices, so we’ll go to that for the first time this year, and what’s neat about it is they’re really promoting young investigators. Each grant can bring up to eight people, the our hope is that we will have the investigators funded by the pilot projects attend next year, giving those folks the opportunity to present and talk to program officers with the NIH and develop a pipeline of investigators committed to studying women’s health and sex as a biological variable.” Sullivan is also looking to designate some of her summer graduate and undergraduate research positions to the project beginning next summer. “The Graduate School already has a summer program to support undergraduates that we will be able to piggyback off of. We have set aside five slots in that program for this that will go to students studying the sex as a biological variable, and the applications for that program, STAR, is already open,” Sullivan said. “We’re also planning a symposium in collaboration with the Physiology Department in April 2024. This is an annual event sponsored by the department, and this year they selected sex differences as the topic, so we are hoping to help increase exposure and attendance.” Looking to know more about the amazing research happening at Augusta? To connect with Jennifer Sullivan, simply click on her icon ow to arrange an interview today.

J.S. Held Announces the First Global Consulting Company Chief Intellectual Property Officer
Global consulting firm J.S. Held proudly announces the appointment of intellectual property (IP) expert James E. Malackowski as the first Chief Intellectual Property Officer (CIPO) of a global consulting company. J.S. Held Chief Executive Officer Lee Spirer observes, “In today's knowledge-based economy, the role of CIPO serves an important strategic and operational role both internally and in support of clients.” Protecting J.S. Held Intellectual Property and Other Intangible Assets J.S. Held experts have developed methodologies, frameworks, proprietary tools, and research that support client work. The CIPO partners across the business to ensure that these intangible assets are identified, protected, and leveraged to benefit the business. “Having dedicated IP leadership will help the company move faster in developing and deploying new methodologies, while ensuring reasonable measures of protecting our innovations,” noted James E. Malackowski. Managing J.S. Held Intellectual Property and Other Intangible Assets J.S. Held maintains a robust portfolio of patents including a “System and Method for Financing an Insurance Transaction”, trademarks, data, trade secrets, and other proprietary technologies that support client work. “As CIPO, I intend to partner with company leadership and our professional experts across the globe to manage and monetize the many patent, trademark, data, and other proprietary assets that set J.S. Held apart among our competitors, benefitting clients and our investors,” added James E. Malackowski. Industry’s Most Comprehensive Global Intellectual Property Consulting Group Ocean Tomo, a part of J.S. Held, is rooted in an expansive understanding of intellectual property (IP) value and risk, providing a foundation of Expertise for the Innovation Economy™. Built upon more than three decades of experience assessing IP in the most rigorous of venues - state, federal, and international courts, Ocean Tomo clients benefit from continuous feedback between litigation economic damage outcomes, transaction pricing, capital market valuations, debt financing terms, equity assessments, and deep technical insight. The team possesses the most comprehensive and market-tested understanding of IP value. Financial, market, and technical experts uniquely understand the contributory value of patented inventions, know-how, brands, and copyrights that permeate every business, viewing IP not simply as an isolated asset, but as an integral component of enterprise value. Multidimensional Intellectual Property-Informed Experts Benefit J.S. Held Clients Intellectual property expertise permeates the global organization. Beyond the expertise within J.S. Held’s dedicated IP practice Ocean Tomo, a part of J.S. Held, multidisciplinary experts across J.S. Held combine intellectual property expertise to core specializations, including: • Artificial Intelligence (AI) • Business Intelligence • Construction Advisory • Enterprise Risk Management • Fraud Investigations • Forensic Accounting • Insurance Claims Consulting • Restructuring, Turnaround, Receivership, and Bankruptcy Tangible and Intangible Asset Value Understanding The depth and breadth of J.S. Held’s work in the property and casualty insurance market and Ocean Tomo’s work across all forms of intellectual property and other intangible assets uniquely combine to create a strong foundation in risk assessment, data analysis, global awareness, regulatory compliance, technological adaptability, and risk mitigation. Collectively, these skills better equip J.S. Held experts to assess business risk across diverse geographies, geopolitical landscapes, regulatory frameworks, and technological advancements for the benefit of our clients. Learn more about the new J.S. Held Chief Intellectual Property Officer, James E. Malackowski: Looking to know more or connect with James E. Malackowski? Simply click on the expert's icon now to arrange an interview today. For any other media inquiries - contact : Kristi L. Stathis, J.S. Held +1 786 833 4864 Kristi.Stathis@JSHeld.com

5 Reasons "Expertise Marketing" Programs Fail.
As a company dedicated to “Expertise Marketing” we work with some of the largest organizations from higher education and healthcare, to top global corporate brands. What these organizations have in common are smart, educated professionals…and a lot of them. The types of individuals that would be valuable ambassadors, true thought leaders, helping you deliver on your organization’s reputational and revenue goals. Instinctively marketing and communications teams recognize the intrinsic value of this human capital and have created a variety of “Thought Leadership” and “Expert Marketing and Directory” initiatives. The overriding objective is how to best connect their experts to audiences that matter. Seeking opportunities ranging from acting as media sources to event speakers to providing a valuable entry-point for research and business collaboration, even lead generation. To execute on this goal, one of the most effective approaches, and starting points for any expertise marketing program starts with better profiling their experts and related insights on their website. Building out and leveraging this expert content is at the core of most expertise marketing efforts. Despite the promises these web initiatives offer, most programs don’t deliver organizations the results they were hoping for. Success most often has nothing to do with how smart your people are. Some of the largest organizations with deep rosters of expertise fail where smaller organizations consistently punch above their weight. When creating an expertise presence on your website there are important areas to consider. The following represents the top 5 reasons many expertise marketing programs fail and how to maximize your success. Reason #1 You’re missing critical team members There is no “going it alone” when starting a program like this. Having the following individuals onboard at the start is crucial. Don't worry, these aren't all full-time resources by any means. As your program progresses, these individuals may come in and out in terms of importance, but having access to them over the lifetime of your program will positively impact your success. At the core, you need access to the following individuals. Program Champion - Having a senior leader as a champion is pretty much table stakes for any successful company-wide initiative such as this. Someone who can articulate to others, both up and down in the organization as to how this initiative fits into the broader long-term goals of the organization is imperative. Failure to establish this individual upfront puts your program's future at the whim of shifting priorities and budget cuts. Marketing/Communications - You need someone with ongoing responsibility for maintaining and promoting your roster of experts and their content. This ensures your most relevant experts are showcased at the right time to meet the changing demands of your audiences and the news cycle. Digital/Web - You need someone with the keys to the website/CMS. Ensure you have connections to people who control not only your small area of the website such as a newsroom or department level webpages but also those that have access to the layouts and navigation of the broader website. The latter is important as it helps prevent your expert content from combing isolated and disconnected from the rest of your website. IT - The level of involvement of IT is highly dependent on how you’re looking to implement your expert content on your website. By leveraging a variety of content implementation tools from simple "cut and paste" embeds to WordPress plugins you can severely limit the necessity to involve IT. However, depending on your budget and goals, IT can leverage a platform's API, accessing advanced layouts and functionality, including integrating with other systems your organization may already be using. Engaged Experts - Last but not least, having your experts on board is critical. By properly communicating upfront and ongoing with your experts around the goals of the program, you're helping ensure your content best represents the talents that lie within. We realize it is often difficult and sometimes cost-prohibitive to assemble such a team. It is important if you don’t have access to all these members in-house that you access them through an external partner's professional services offerings. This could include assisting with building out content such as profiles and posts or providing technical assistance in integrating this content into your website. Reason #2 You’re relying too much on IT for implementation or updating. To be successful long term, it is important that key owners of the expertise marketing program feel empowered to take control of their expert content. From creation to ongoing management, those with marketing communications roles and others closest to their organization’s expertise need the flexibility to update content in real-time to remain relevant and up-to-date. Being able to quickly log into an external platform that syncs content with your website is key. It eliminates the need for special access to your CMS or the possible requirement for IT to be in control of your updates. It also allows for a mix of individual expert and administrator access providing the highest level of flexibility. Often left out in IT-focused builds is how you will effectively handle inquiries. Simply showing emails and phone numbers is a recipe for missed opportunities (and SPAM) as these experts are some of the most time-constrained individuals in your organization. Ensuring you have access to a customizable workflow feature is essential in ensuring your organization doesn't miss potential time-sensitive inquiries. When working with IT to implement an Expertise Marketing Program on your website, you will often be presented with a “we’ll build it for you option” vs using a purpose-built platform. Understanding the tradeoffs of this approach is critical. One of the greatest benefits of using a SaaS platform, besides costs, is that you constantly have the most up-to-date software, with the latest features and functionality to best showcase your expertise. To learn more, download the “True Costs of DIY” to better understand the tradeoffs and functional requirements needed for success. Reason #3 Your expert content is siloed, one-dimensional, and rarely updated. This is by far one of the biggest reasons programs fail. Well, it's actually a number of reasons, but it all relates back to how your content will be perceived and ultimately drive connections with interested audiences. By addressing the following you'll present not only better but more easily discoverable expert content that drives inquiries. You have boring, not engaging profiles for your experts - Before people feel comfortable reaching out they need a good sense of the person. Profiles that lack media assets such as video, publications and even podcasts are one-dimensional. Furthermore, showcasing past media and event appearances provides an enhanced level of credibility. Focused solely on a directory & profiles - Your expertise is more than just showcased through a profile found in a directory. Adding long-form posts where experts can share their insights and even expert focussed Q&A (download report on "The Power of Q&A") provides audiences additional ways to connect with your experts. Ensuring all these additional assets connect back to your profiles provides more insight into the person behind the expertise. No main website navigation - Despite adding menu navigation on a specific web page, such as a newsroom or About Us page, most organizations neglect to add navigation to their main website’s menu structure. You can never assume visitors will know where this content resides. We recommend multiple links in both headers and footers to your expert content. Names such as “Find Experts”, “Media Sources” or “Research Experts” are some of the most common, accessible from overall menu items like “About Us”, “News” or “Research”. Expert content stuck to one small area of your website - If you restrict your expert content to just one area, you’re just making discovery that much harder and limiting exposing the breadth of expertise you have in-house. Highlight your experts and expertise on your homepage or in key sections of your website. Refine your experts and their insights found in posts or Q&A by tagging them based on specific topics and showcasing just those experts in various areas of your website. Using a dedicated SaaS platform means that when you update content it updates everywhere, making changes quick and easy. Expert content never gets updated - This is a big issue for organizations that build in-house or through their CMS. Visitors can quickly understand that the content isn’t fresh and it reflects poorly on the individual and the organization as a whole. The key to ensuring content is maintained is to provide multiple access capabilities where admins (internal or external) and the experts can maintain the content. Failure to respond in a timely manner to inquiries - Displaying content that exposes phone numbers and emails of your experts is not the best approach...both from a privacy and timely communications standpoint. Without an advanced inquiry workflow that alerts multiple members of your team, you risk missing out on time-sensitive requests such as those from journalists. Reason #4 You haven’t considered everything needed to win the SEO game. Building out content on the web without having a plan for how external and internal search engines will interact with your pages is a big mistake. Organic search can play a big role in discovery leading to valuable opportunities. Before you consider your new expert content pages ready, ensure you've taken into account the following. Proper Meta Data - Do your expert profile pages have dynamically created titles, descriptions and keywords that automatically adjust to changes in areas such as an individual's expertise? Schema Data - Do you have proper schema tags that indicate to Google and other search engines the type of content displayed as well as the credibility of both the individual and organization behind it. Sitemaps - Have you ensured all your pages have been added to your sitemap. Is it automatically updated when new experts or pieces of expert content are added? Google Search Console - Are you pushing pages directly to Google by requesting important new content is updated in the search index. For more info on better SEO read my Spotlight "Why Expertise Ranks Higher". Reason #5 You’re not doing enough to actively promote your expertise… a “they’ll just find us” approach usually fails. It's like owning a Porsche and leaving it in the garage…pretty to look at but you’re not realizing its full potential. Simply putting your expert content on a web page is only the start. Successful organizations actively distribute these assets, sharing links to profiles and other content elements like news posts or Q&A in a variety of ways. Social Media Channels - They start by promoting these assets on their social media channels, from their Twitter feeds to Facebook and LinkedIn posts. Media Distribution Software - Whether it is systems like Cision or Meltwater, including links to expert profiles and related content when reaching out to journalists adds a layer of depth to your pitches. Press Releases - Every time you reference your organization's expertise, include links to additional content and individual experts for more insights and pathways to connect with real people. It sounds like a lot, but with a bit of planning and some ongoing maintenance, a properly constructed expertise marketing program can deliver incredible results for many years. To be successful it's more than just firing up a few new web pages. However, with the advent of specialized platforms specifically designed for these programs, and a bit of guidance, it is easier than ever to create an expert content footprint on your website and deliver valuable connections for your organization.
Julian Ku Examines China’s Role in New International Mediation Agreement
Hofstra Law Professor Julian Ku provided legal insights to Newsweek on the Convention on the Establishment of the International Organization for Mediation agreement that was signed by China and 32 other countries. The organization stands as the first of its kind, dedicated solely to facilitating mediation between nations.

Why Your Experts Might Not Show Up in Google AI Overviews — And How to Fix It
The way we find expert information online is changing fast. With the rise of Google’s AI-generated overviews (formerly called Search Generative Experience), the top spot on the search page no longer goes to the highest-ranking blue link. Instead, AI now summarizes answers using a blend of machine learning, structured data, and trust signals—pulling directly from a variety of select sources across the web. If institutions—whether academic, healthcare, corporate or others—aren't aligning its expert content with these new rules of discovery, your experts may be left out of the conversation altogether. Don't miss being featured in media stories, invited to speak at events, or approached for business and collaboration opportunities. This is the moment to double down on structured data and transparent authorship—because AI-first search is rewarding expert clarity, not just content volume. The following provides a quick breakdown as to how AI Search, Google’s EEAT principles, and Schema.org structured data work together—and what you can do to ensure your expert content...and your experts, gets surfaced, cited, and trusted. What Is EEAT and Why It Matters in AI Search EEAT stands for Experience, Expertise, Authoritativeness, and Trustworthiness—the core framework Google uses to evaluate whether content is reliable and deserves to rank, especially in high-stakes areas like health, education, and finance. In AI-powered summaries, Google doesn’t just look at keywords—it looks for: Real people with demonstrable credentials Clear affiliations with reputable institutions Consistent authorship and transparency Trust signals like citations, bios, and professional history EEAT in Action: Why Schema Markup Is Your AI SEO Power Tool EEAT signals work best when they’re machine-readable—that’s where Schema.org structured data comes in. It acts as a translator between your content and Google’s AI. Schema tags are pieces of structured data that help search engines understand the content and context of your web pages. They translate human-readable information—like author names, job titles, and article types—into machine-readable signals that boost visibility AI overviews and search results. Implementing Schema helps ensure your expert content is eligible for inclusion in AI overviews. Key schema types include: {Person} – for expert bios {ScholarlyArticle}, {Article}, {FAQ} – for authored content {Organization}, {MedicalOrganization}, {EducationalOrganization} – to establish credibility {sameAs} – to reinforce expertise by connecting external profiles (LinkedIn, ORCID, Google Scholar) Schema in Action: AI Overviews Favor Structured, Credible Expert Content Google’s AI overviews are designed to synthesize trustworthy sources—not just surface-level blog posts or SEO-churned pages. That means expert content that is: Authored by named individuals with clear credentials Structured for readability and machine parsing Linked to institutional authority and trust domains If your experts don’t meet these criteria—or if Google’s crawlers can’t understand the relationships between person, organization, and content—your insights may never reach the surface of the AI summary box. How ExpertFile Optimizes for AI-Driven Search AI search is no longer just about keywords—it’s about credibility, structure, and clarity. Institutions that invest in properly structured expert content will not only rank better—they’ll become the source quoted in the next generation of search. ExpertFile is purpose-built to maximize visibility and trust in this new era of AI search. Here’s how: Structured Expert Profiles: Every expert has a dedicated page with rich Person schema, bios, credentials, affiliations, and publication history. Schema-Tagged Content: Articles, media spotlights, and FAQs are marked up using Schema.org types like ScholarlyArticle, FAQPage, and Article. Institutional Credibility: Profiles are embedded within .edu, .org, or corporate domains—reinforcing trust with Google’s algorithms. Cross-Linked Authority: Integration with Google Scholar, LinkedIn, and ORCID ensures a 360° trust profile across the web. Mobile-Ready & Indexed: ExpertFile content is fully indexable and distributed across web and mobile platforms—supporting discoverability everywhere AI pulls from. With ExpertFile, your experts are not just listed—they’re positioned, structured, and ready for the AI spotlight. Learn more about how ExpertFile helps organization's benefit in the new era of AI.

Google's New AI Overviews Isn’t Just Another Search Update
Google's recent rollout of AI Overviews (previously called “Search Generative Experience”) at its annual developer conference is being hailed as the biggest transformation in search since the company was founded. This isn’t a side project for Google — it fundamentally alters how content gets discovered, consumed, and valued online. If you're in marketing, PR, content strategy, or run a business that depends on online visibility, this requires a fundamental shift in your thinking. What Is AI Overviews? Instead of showing users a familiar list of blue links and snippets, Google now uses artificial intelligence to generate a summary answer at the very top of many search results pages. This AI-generated box pulls together content from across the web and tries to answer the user’s question instantly—without requiring them to click through to individual websites. Here’s what that looks like: You type in a question like “What are the best strategies for handling a media crisis?” Instead of just links, you see a big AI-generated paragraph with summarized strategies, possibly quoting or linking to 3-5 sources—some of which might not even be visible unless you scroll or expand the summary. Welcome to the new digital gatekeeper. Elizabeth Reid, VP of Search at Google states "Our new Gemini model customized for Google Search brings together Gemini’s advanced capabilities — including multi-step reasoning, planning and multimodality — with our best-in-class Search systems. Let's breakdown this technobabble. Think of Gemini as the brain behind Google’s search engine that’s now: Even More Focused on User intent For years, SEO strategies were built around guessing and gaming the right keywords: “What exact phrase are people typing into Google?” That approach led to over-optimized content — pages stuffed with phrases like “best expert speaker Boston cleantech” — written more for algorithms than actual humans. But with Google Gemini and other AI models now interpreting search queries like a smart research assistant, the game has changed entirely. Google is no longer just matching phrases — it’s interpreting what the user wants to do and why they’re asking. Here’s What That Looks Like: Let’s say someone searches: “How do I find a reputable expert on fusion energy who can speak at our cleantech summit?” In the old system, pages that mentioned “renewable energy,” “expert,” and “speaker” might rank — regardless of whether they actually helped the user solve their problem. Now Google more intuitively understands: • The user wants to evaluate credibility • The user is planning an event • The user needs someone available to speak • The context is likely professional or academic If your page simply has the right keywords but doesn’t send the right signals — you’re invisible. Able to plan ahead Google and AI search platforms now go beyond just grabbing facts. They string together pieces of information to answer more complex, multi-step queries. In traditional search, users ask one simple question at a time. But with multi-step queries, users are increasingly expecting one search to handle a series of related questions or tasks all at once — and now Google can actually follow along and reason through those steps. So imagine you’re planning a conference. A traditional search might look like: "Best conference venues in Boston” But a multi-step query might be: “Find a conference venue in Boston with breakout rooms, check availability in October, and suggest nearby hotels with group rates.” This used to require three or four different searches, and you’d piece it together yourself. Now Google can handle that entire chain of related tasks, plan the steps behind the scenes, and return a highly curated answer — often pulling from multiple sources of structured and unstructured data. Even Better at understanding context Google now gets the difference between ‘a speaker at a conference’ and ‘a Bluetooth speaker’ — because it understands what you mean, not just what you type.” In the past, Google would match keywords literally. If your page had the word “speaker,” it might rank for anything from event keynotes to audio gear. That’s why so many search results felt off or required extra digging. Now Google reads between the lines. It understands that “conference speaker” likely refers to a person who gives talks, possibly with credentials, experience, and a bio. And that “Bluetooth speaker” is a product someone might want to compare or buy. Why this matters for marketers: If you’re relying on vague or generic content — or just “keyword-stuffing” — your pages will fall flat. Google is no longer fooled by superficial matches. It wants depth, clarity, and specificity. Reads More Than Just Text Google now processes images, videos, charts, infographics, and even audio — and uses that multimedia information to answer search queries more completely. This now means that your content isn’t just being read like a document — it’s being watched, listened to, and interpreted like a human would. For example: • A chart showing rising enrollment in nursing programs might get picked up as supporting evidence for a story about healthcare education trends. • A YouTube video of your CEO speaking at a conference might be indexed as proof of thought leadership. • An infographic explaining how your service works could surface in an AI-generated summary — even if the keyword isn’t mentioned directly in text. Ignoring multimedia formats? Then, your competitors’ visual storytelling could be outperforming your plain content. Because you're not giving Google the kind of layered, helpful content that Gemini is now designed to highlight. Why This Matters There's a big risk here. Marketers who ignore these developments are in danger of becoming invisible in search. Your old SEO tricks won’t work. Your content won’t appear in AI summaries. Your organization won’t be discovered by journalists, customers, or partners who now rely on smarter search results to make decisions faster. If you’re in communications, PR, media relations, or digital marketing, here’s the key message. You are no longer just fighting for links. You need to fight to be included in the Google AI summary itself at the top of search results - that's the new #1 goal. Why? Journalists can now find their answers before ever clicking on your beautifully written news page. Prospective students, donors, and customers will often just see the AI’s version of your content. Your brand’s visibility now hinges on being seen as “AI-quotable.” If your organization isn’t optimized for this new AI-driven landscape, you risk becoming invisible at the very moment people are searching for what you offer. How You Can Take Action (and Why Your Role Is More Important Than Ever) This isn’t just an IT or SEO problem. It’s a communications strategy opportunity—and you are central to the solution. What You Can Do Now to Prepare for AI Overviews 1. Get Familiar with How AI “Reads” Your Content AI Overviews pull content from websites that are structured clearly, written credibly, and explain things in simple language. Action Items: Review your existing content: Is it jargon-heavy? Outdated? Lacking expert quotes or explanations? Then, it's time to clean house. 2. Collaborate with your SEO and Web Teams Communicators and content creators now need to work hand-in-hand with technical teams. Action Items: Check your pages to see if you are using proper schema markup. Are you creating topic pages that explain complex ideas in simple, scannable formats? 3. Showcase Human Expertise AI values content backed by real people—especially experts with credentials. Action Items: Make sure your expert profiles are up to date. Make sure you continue to enhance them with posts, links to media coverage, short videos, images and infographics that highlight the voices behind your brand and make you stand out in search. 4. Don’t Just Publish—Package AI favors content that it can easily digest and display such as summary paragraphs, FAQs, and bold headers that provide structure for search engines. This also makes your content more scannable and engaging to humans. Action Items: Repurpose your best content into AI-friendly formats: think structured lists, how-tos, and definitions. 5. Monitor Your Presence in AI Overviews Regularly search key topics related to your organization and see what shows up. Action Items: Is your content featured? If not, whose is—and identify what they doing differently. A New Role for Communications: From Media Pitches to Machine-Readable Influence This isn’t the end of communications as we know it—it’s an evolution. Your role now includes helping your organization communicate clearly to machines as well as to people. Think of it as “PR for the algorithm.” You’re not just managing narratives for the public—you’re shaping what AI systems say about you and your brand. That means: • Ensuring your best ideas and experts are front and center online. • Making complex information simple and quotable. • Collaborating cross-functionally like never before. Final Thought: AI Search Rewards the Prepared Google’s new AI Overviews are here. They’re not a beta test. This is the future of search, and it’s already rolling out. If your institution, company, or nonprofit wants to be discovered, trusted, and quoted, you can no longer afford to ignore how AI interprets your online presence. Communications and media professionals are now at the front lines of discoverability. And the best way to lead is to act now, work collaboratively, and elevate your role in this new era of search. Want to see how leading organizations are getting ahead in the age of AI search? Discover how ExpertFile is helping corporations, universities, healthcare institutions and industry associations transform their knowledge into AI-optimized assets — boosting visibility, credibility, and media reach. Get your free download of our app at www.expertfile.com