Experts Matter. Find Yours.
Connect for media, speaking, professional opportunities & more.
AU research team awarded $4.4 million American Heart Association grant
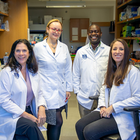
A research team at Augusta University, led by Jennifer C. Sullivan, PhD, has secured a $4.4 million grant from the American Heart Association to study the risk factors for cardiovascular and kidney diseases and how they impact women. Sullivan’s research center, “Disruptions in cardiorenal free fatty acid metabolism in Cardiovascular Kidney Metabolic Syndrome,” is part of a larger $15 million project titled “Strategically Focused Research Network on Cardiovascular Kidney Metabolic Syndrome: Heterogeneity in Women.” The overarching AHA project is aimed at learning why women may be more likely to develop cardiovascular and kidney diseases due to certain unique risk factors and life stages. Research teams from Massachusetts General Hospital and The Ohio State University were also chosen. “I think this is a huge step for Augusta University as we continue to distinguish ourselves and the research that we have here focused on the health of women,” said Sullivan, dean of The Graduate School. “This grant is particularly impactful as we look to advance and improve the health of women, not just in Georgia, but for the entire country.” According to the Healthy Georgia Report, produced by AU’s School of Public Health, Georgia has the 23rd highest rate of obesity in the United States. Among the women living in the state, 38.3% of them, as well as 37.5% of people living in rural areas, suffer from obesity. “It’s great that we are able to represent the state of Georgia because our state has such a high prevalence for obesity rates,” said Sullivan, who is the director of AU’s SCORE project “Improving awareness of women with hypertension: ROAR (Rural, Obese, At Risk).” “It’s important for us to understand that different populations have distinct needs. You can’t talk about a one-size-fits-all approach to health. This is really about trying to understand how different groups are impacted.” Each center is comprised of three teams, as well as a training component and an area partner. Together, they will explore obesity’s lifetime impact on CKM syndrome through three projects. CKM syndrome is a clinical term that describes the combined health effects of heart disease, kidney disease, diabetes and obesity, which puts people at high risk for heart attack, stroke and heart failure. According to the American Heart Association’s 2025 Heart Disease and Stroke Statistics, about 1 in 3 U.S. adults has at least three components of CKM syndrome, which include high blood pressure, abnormal cholesterol, high blood glucose (sugar), impaired kidney function and excess body weight. The first project is led by Daria Ilatovskaya, PhD, and Justine Abais-Battad, PhD, and will look at aging and Western diet-induced CKMS mechanisms in obesity. Ilatovskaya is an associate professor and the graduate program director for the Doctor of Philosophy in Physiology program, and Abais-Battad is an assistant professor in the Department of Physiology with the Medical College of Georgia at Augusta University. The second component, led by Jessica Faulkner, PhD, an assistant professor in MCG’s Physiology department, will study obesity-associated mechanisms of CKMS in pregnancy. The third project, led by Stephen Coughlin, PhD, with Marlo Vernon, PhD, is looking at CKMS epidemiology, associations with obesity, CVD/CKD. Coughlin is the program director for the Master of Science in Epidemiology and professor of epidemiology in the School of Public Health’s Department of Biostatistics, Data Science, and Epidemiology, while Vernon is an associate professor with MCG’s Georgia Prevention Institute and SPH’s Department of Community and Behavioral Health Sciences. Additionally, the team will talk to women and health care providers from a variety of backgrounds and experiences to assess current knowledge and interest levels in heart health and use that information to develop programs that may help treat and prevent disease. There is also a training director, Alison Kriegel, PhD, a professor in the Department of Physiology, and a core director, Guido Verbeck, PhD, chair and professor of the Department of Chemistry and Biochemistry in the College of Science and Mathematics. “We have a strong blend of clinical epidemiology and basic science, as well as a training component, which we will fill with post-doctoral fellows,” Sullivan said. “Dr. Ilatovskaya, Dr. Faulkner, Dr. Abais-Battad and Dr. Vernon are all a part of our ROAR grant, and, while this isn’t directly related to that program, it allowed us to demonstrate how we are already well positioned to work together to amplify our ability and increase awareness about the importance of the health of women.” The team has over 50 collaborative papers and has secured more than $13 million in collaborative funding to advance the health of women. They also all have experience training fellows and students to continue to expand their reach. “We already have a lot of the infrastructure in place for this kind of cross-disciplinary project, so we leaned very heavily into our connections and the expertise we have here at Augusta University. It’s set up very similar to our ROAR program, so this is something that was really organic in nature,” Sullivan said. The American Heart Association has invested almost $300 million to establish 18 Strategically Focused Research Networks, each aimed at addressing a key strategic issue identified by the association’s volunteer Board of Directors. Prior networks have been studying a wide variety of important topics including, but not limited to, prevention, hypertension, the health of women, heart failure, obesity, vascular disease, atrial fibrillation, arrhythmias/sudden cardiac death, cardiometabolic health/type 2 diabetes, health technology, cardio-oncology, the biological impact of chronic psychosocial stress and the role of inflammation in cardiovascular health. Each network centers around scientific knowledge and knowledge gaps, prevention, diagnosis and treatment of the key research topic. Three to six research centers make up each network, bringing together investigators with expertise in basic, clinical and population/behavioral health science to find new ways to diagnose, treat and prevent heart disease and stroke. Funding scientific research and discovery through initiatives like these awards is a cornerstone of the century-old American Heart Association’s lifesaving mission. The association has now funded more than $5.9 billion in cardiovascular, cerebrovascular and brain health research since 1949, making it the single largest non-government supporter of heart and brain health research in the United States. New knowledge resulting from this funding continues to save lives and directly impact millions of people in every corner of the U.S. and around the world. Looking to know more about the amazing research happening at Augusta? To connect with Dr. Sullivan, simply click on her icon to arrange an interview today.

Virtual reality training tool helps nurses learn patient-centered care
University of Delaware computer science students have developed a digital interface as a two-way system that can help nurse trainees build their communication skills and learn to provide patient-centered care across a variety of situations. This virtual reality training tool would enable users to rehearse their bedside manner with expectant mothers before ever encountering a pregnant patient in person. The digital platform was created by students in Assistant Professor Leila Barmaki’s Human-Computer Interaction Laboratory, including senior Rana Tuncer, a computer science major, and sophomore Gael Lucero-Palacios. Lucero-Palacios said the training helps aspiring nurses practice more difficult and sensitive conversations they might have with patients. "Our tool is targeted to midwifery patients,” Lucero-Palacios said. “Learners can practice these conversations in a safe environment. It’s multilingual, too. We currently offer English or Turkish, and we’re working on a Spanish demo.” This type of judgement-free rehearsal environment has the potential to remove language barriers to care, with the ability to change the language capabilities of an avatar. For instance, the idea is that on one interface the “practitioner” could speak in one language, but it would be heard on the other interface in the patient’s native language. The patient avatar also can be customized to resemble different health stages and populations to provide learners a varied experience. Last December, Tuncer took the project on the road, piloting the virtual reality training program for faculty members in the Department of Midwifery at Ankara University in Ankara, Turkey. With technical support provided by Lucero-Palacios back in the United States, she was able to run a demo with the Ankara team, showcasing the UD-developed system’s interactive rehearsal environment’s capabilities. Last winter, University of Delaware senior Rana Tuncer (left), a computer science major, piloted the virtual reality training program for Neslihan Yilmaz Sezer (right), associate professor in the Department of Midwifery, Ankara University in Ankara, Turkey. Meanwhile, for Tuncer, Lucero-Palacios and the other students involved in the Human-Computer Interaction Laboratory, developing the VR training tool offered the opportunity to enhance their computer science, data science and artificial intelligence skills outside the classroom. “There were lots of interesting hurdles to overcome, like figuring out a lip-sync tool to match the words to the avatar’s mouth movements and figuring out server connections and how to get the languages to switch and translate properly,” Tuncer said. Lucero-Palacios was fascinated with developing text-to-speech capabilities and the ability to use technology to impact patient care. “If a nurse is well-equipped to answer difficult questions, then that helps the patient,” said Lucero-Palacios. The project is an ongoing research effort in the Barmaki lab that has involved many students. Significant developments occurred during the summer of 2024 when undergraduate researchers Tuncer and Lucero-Palacios contributed to the project through funding support from the National Science Foundation (NSF). However, work began before and continued well beyond that summer, involving many students over time. UD senior Gavin Caulfield provided foundational support to developing the program’s virtual environment and contributed to development of the text-to-speech/speech-to-text capabilities. CIS doctoral students Fahim Abrar and Behdokht Kiafar, along with Pinar Kullu, a postdoctoral fellow in the lab, used multimodal data collection and analytics to quantify the participant experience. “Interestingly, we found that participants showed more positive emotions in response to patient vulnerabilities and concerns,” said Kiafar. The work builds on previous research Barmaki, an assistant professor of computer and information sciences and resident faculty member in the Data Science Institute, completed with colleagues at New Jersey Institute of Technology and University of Central Florida in an NSF-funded project focused on empathy training for healthcare professionals using a virtual elderly patient. In the project, Barmaki employed machine learning tools to analyze a nursing trainee’s body language, gaze, verbal and nonverbal interactions to capture micro-expressions (facial expressions), and the presence or absence of empathy. “There is a huge gap in communication when it comes to caregivers working in geriatric care and maternal fetal medicine,” said Barmaki. “Both disciplines have high turnover and challenges with lack of caregiver attention to delicate situations.” UD senior Rana Tuncer (center) met with faculty members Neslihan Yilmaz Sezer (left) and Menekse Nazli Aker (right) of Ankara University in Ankara, Turkey, to educate them about the virtual reality training tool she and her student colleagues have developed to enhance patient-centered care skills for health care professionals. When these human-human interactions go wrong, for whatever reason, it can extend beyond a single patient visit. For instance, a pregnant woman who has a negative health care experience might decide not to continue routine pregnancy care. Beyond the project’s potential to improve health care professional field readiness, Barmaki was keen to note the benefits of real-world workforce development for her students. “Perceptions still exist that computer scientists work in isolation with their computers and rarely interact, but this is not true,” Barmaki said, pointing to the multi-faceted team members involved in this project. “Teamwork is very important. We have a nice culture in our lab where people feel comfortable asking their peers or more established students for help.” Barmaki also pointed to the potential application of these types of training environments, enabled by virtual reality, artificial intelligence and natural language processing, beyond health care. With the framework in place, she said, the idea could be adapted for other types of training involving human-human interaction, say in education, cybersecurity, even in emerging technology such as artificial intelligence (AI). Keeping people at the center of any design or application of this work is critical, particularly as uses for AI continue to expand. “As data scientists, we see things as spreadsheets and numbers in our work, but it’s important to remember that the data is coming from humans,” Barmaki said. While this project leverages computer vision and AI as a teaching tool for nursing assistants, Barmaki explained this type of system can also be used to train AI and to enable more responsible technologies down the road. She gave the example of using AI to study empathic interactions between humans and to recognize empathy. “This is the most important area where I’m trying to close the loop, in terms of responsible AI or more empathy-enabled AI,” Barmaki said. “There is a whole area of research exploring ways to make AI more natural, but we can’t work in a vacuum; we must consider the human interactions to design a good AI system.” Asked whether she has concerns about the future of artificial intelligence, Barmaki was positive. “I believe AI holds great promise for the future, and, right now, its benefits outweigh the risks,” she said.

Babies whose mothers took kale or carrot capsules when pregnant responded more favourably to these smells The research shows that the process of developing food preferences begins in the womb, much earlier than previously thought The research follows up on an earlier study Babies show positive responses to the smell of foods they were exposed to in the womb after they are born, according to a new study. The findings, led by Durham University, UK, could have implications for understanding how healthy eating habits might be established in babies during pregnancy. The research included scientists from Aston University, UK, and the Centre national de la recherche scientifique (CNRS) and University of Burgundy, France. It is published in the journal Appetite. Researchers analysed the facial expressions of babies who had been repeatedly exposed to either kale or carrot in the womb after birth. Newborns whose mothers had taken carrot powder capsules when pregnant were more likely to react favourably to the smell of carrot. Likewise, babies whose mothers had taken kale powder capsules while pregnant reacted more positively to the kale scent. Research co-lead author and supervisor Professor Nadja Reissland, of the Fetal and Neonatal Research Lab, Department of Psychology, Durham University, said: “Our analysis of the babies’ facial expressions suggests that they appear to react more favourably towards the smell of foods their mothers ate during the last months of pregnancy. Potentially this means we could encourage babies to react more positively towards green vegetables, for example, by exposing them to these foods during pregnancy. “In that respect, the memory of food the mother consumes during pregnancy appears to establish a preference for those smells and potentially could help to establish healthy eating habits at a young age.” This study is a follow-up to a 2022 research paper where the researchers used 4D ultrasound scans at 32 and 36 gestational weeks to study foetal facial expressions after their pregnant mothers had ingested a single dose of either 400mg of carrot or kale capsules. Foetuses exposed to carrot showed more “laughter-face” responses while those exposed to kale showed more “cry-face” responses. For the latest study, the researchers followed up 32 babies from the original research paper – 16 males and 16 females – from 36 weeks gestation until approximately three weeks after birth. Mothers consumed either carrot or kale capsules every day for three consecutive weeks until birth. When the babies were about three weeks old, the research team tested newborns’ reactions to kale, carrot, and a control odour. Separate wet cotton swabs dipped in either carrot or kale powders, or water as the control, were held under each infant’s nose and their reaction to the different smells was captured on video. The babies did not taste the swabs. Scientists then analysed the footage to see how the newborns reacted and compared these reactions with those seen before the babies were born to understand the effects of repeated flavour exposure in the last trimester of pregnancy. The research team found that, from the foetal to newborn period, there was an increased frequency in “laughter-face” responses and a decreased frequency in “cry-face” responses to the smell the babies had experienced before birth. Humans experience flavour through a combination of taste and smell. In foetuses, this happens through inhaling and swallowing the amniotic fluid in the womb. Research co-lead author Dr Beyza Ustun-Elayan carried out the research while doing her PhD at Durham University. Dr Ustun-Elayan, who is now based at the University of Cambridge, said: “Our research showed that foetuses can not only sense and distinguish different flavours in the womb but also start learning and establish memory for certain flavours if exposed to them repeatedly. This shows that the process of developing food preferences begins much earlier than we thought, right from the womb. By introducing these flavours early on, we might be able to shape healthier eating habits in children from the start.” The researchers stress that their findings are a baseline study only. They say that longer follow-up studies are needed to understand long-term impacts on child eating behaviour. They add that further research would also need to be carried out on a larger group of infants, at different points in time. They say that the absence of a control group not exposed to specific flavours makes it challenging to fully disentangle developmental changes in the babies from the effects of repeated flavour exposure. Future research should also factor in post-birth flavour experiences, such as some milk formulas known to have a bitter taste, which could impact babies’ responses to the smell of bitter and non-bitter vegetables. The research involved the children of white British mothers, and the researchers say that future studies should be widened to explore how different cultural dietary practices might influence foetal receptivity to a broader array of flavours. Research co-author Professor Jackie Blissett, at Aston University’s School of Psychology, said: “These findings add to the weight of evidence that suggests that flavours of foods eaten by mothers during late pregnancy are learnt by the foetus, preparing them for the flavours they are likely to experience in postnatal life.” Research co-author Professor Benoist Schaal, National Centre for Scientific Research (CNRS)-University of Burgundy, France said: “Foetuses not only detect minute amounts of all types of flavours the mothers ingest, but they overtly react to them and remember them while in the womb and then after birth for quite long times. In this way, mothers have an earlier than early teaching role, as the providers of the infant’s first odour or flavour memories.” Visit https://doi.org/10.1016/j.appet.2025.107891 to read the full research paper in Appetite.

Veronica Chandler’s north Wilmington home is her sanctuary, and it shows. From the soft instrumental music to the scent of lavender to the comfy seats that invite visitors to put up their feet, the message is clear – rest, relax, recharge. Original artwork by Veronica Chandler In this space, Chandler celebrates her rediscovered self, and it’s a journey she shares with all who visit. Part of the cozy feeling in her home comes from the artwork that lines the walls – mostly her own paintings and drawings created over the last six years as she navigates the challenges and triumphs of motherhood and discovers new ways to care for herself and those she loves. After experiencing anxiety, panic attacks and profound depression following the birth of her daughter in 2018, Chandler sought help at the ChristianaCare Center for Women’s Emotional Wellness, where a combination of medication and therapy helped her feel healthier and reconnected. She also returned to a former passion – art. “When I started painting, I found a way of silencing my brain, of calming it down. Being able to just focus on one thing on its own let my body regulate my nervous system,” she said. “I didn’t know what was happening to me. I just felt amazing.” More than ‘baby blues’ Perinatal mood and anxiety disorders are among the most common complications that occur in pregnancy or in the first year after delivery, according to the American College of Obstetricians and Gynecologists. Although many parents experience feelings of anxiety, fatigue and sadness in the first days with a new baby, postpartum depression can occur several months after childbirth. Symptoms are often more severe and can include extreme stress. Despite increased awareness efforts in recent years, perinatal mood and anxiety disorders – including postpartum depression, which occurs in up to 20% of all births – remain underdiagnosed, untreated or undertreated, even though the health impact extends beyond the person giving birth, said Malina Spirito, Psy.D., MEd, director of the Center for Women’s Emotional Wellness. The center opened in 2013 to help patients and their loved ones understand the challenges associated with perinatal mood and anxiety disorders. Since then, the program has tripled the number of clinicians and expanded services to include inpatient and outpatient consultations, ongoing psychotherapy and psychiatric medication management. “Just because we know something is common does not mean we have to put up with it, especially because the effects will be lasting if we don’t address them,” Spirito said. “Perinatal mood disorders have an impact on the overall health of a family. When a mom feels better, the relationships they have with the people around them are better as well.” Breaking the ‘super mom’ stereotype Looking back, Chandler recognizes her struggles with sleeping and anxiety following the birth of her first child may have been signs of postpartum depression. The symptoms went away only to return after her daughter was born two years later. Veronica Chandler sought help from the ChristianaCare Center for Women’s Emotional Wellness for postpartum depression. Caring for herself helped her rediscover her love of creating art. Although overjoyed by her growing family, Chandler deeply missed her mother, who lived in her native Ecuador. Added to those challenges were longer stays in the hospital for Chandler, who had a Caesarean section birth, and for her daughter, who had some minor health issues. In the weeks after giving birth, Chandler battled dizziness caused by anemia. Though exhausted by caring for a newborn, she couldn’t sleep. She constantly felt on edge, and her skin itched without relief. Worried when her symptoms didn’t abate after three months, Chandler’s husband broached the idea of postpartum depression. For Chandler, it was a relief another person noticed something was wrong, but she was scared to think about what might be needed to get better. “I think we’re programmed by our cultures and by our beliefs to think that we need to be ‘super moms’ and give everything we have,” said Chandler, who grew up in Ecuador and moved to the United States after marrying her husband. “I was in such a fog that I didn’t know I could still shine and be happy and content. The default for so many moms is to pour until there’s nothing left.” ‘Rediscovering who I was’ Chandler sought help at the Center for Women’s Emotional Wellness and soon began taking an anti-depressant as part of her treatment. She also saw a therapist to talk about the feelings she was experiencing. “Therapy was such a big part of this whole journey of rediscovering who I was. When you talk and someone listens, you figure things out,” Chandler said. While on a trip to Arizona with a cousin, Chandler discovered kachina dolls, a Native American art form often used to provide guidance to young people and instill the connection between nature and the spirit. The intricately designed images further fueled Chandler’s reignited passion for art. That passion helped Chandler manage the additional challenges brought on by the COVID-19 pandemic when her anxiety and depression resurfaced. Using painting, sculpture and other media, she has examined her own feelings relating to motherhood, family and society. Her work has been featured internationally in Vogue and closer to home in local art galleries. “Some people like to cook, and some people like to write. Art is my creative outlet that allowed me to come back to who I am,” she said. “We all have to release that creativity in some way.” Entering care sooner While the Center for Women’s Emotional Wellness has always focused on pregnant and postpartum patients, it has grown to address mental health needs related to preconception health, including artificial reproductive technology such as in vitro fertilization, Spirito said. The center also sees patients grieving a pregnancy or neonatal loss. More people are thinking about their mental health before they give birth, said Malina Spirito, Psy.D., MEd, director of the ChristianaCare Center for Women’s Emotional Wellness. “One of the most notable observations I’ve seen over the years is that birthing people are entering care sooner. It isn’t uncommon for women to seek out consultation prior to getting pregnant about how to manage their mood disorder should they become pregnant,” said Megan O’Hara, LCSW, a behavioral health therapist with the Center for Women’s Emotional Wellness. “Patients are educating themselves now and expecting their providers to consider their mental health as well as their physical health when getting care.” Women’s mental health care also has become more accessible, said Cynthia Guy, LMSW, MSCC, a women’s health behavioral consultant with the Center for Women’s Emotional Wellness. Behavioral health services are available in every ChristianaCare women’s health practice, including virtual and in-person care. “I can be the bridge connecting the patient with the resources they need to help them manage symptoms and what they are going through,” Guy said. Filling the cup As a result of her own experiences, Chandler teaches classes to help other mothers create their own art as a means of expression. It’s a small way of helping them to fill their own cup. The woman who once hid in her own closet to hide her feelings speaks openly about mental health with the hope people will lose their preconceived ideas about depression and anxiety. “I am so thankful for the journey and the many people I’ve met that have postpartum depression,” she said. “When we talk about what makes the best moms, I think the best mom is a healthy mom who is in balance and harmony.”

ChristianaCare Launches a New Speakers Bureau: Is This the Future of Healthcare Communications?
Only just a few months after their win of an IABC Gold Quill Award (shared with ExpertFile), the ChristianaCare healthcare communications and digital team has once again made major moves to make their organization even more accessible to the community with the launch of their new ChristianaCare Speakers Bureau. As one of the leading healthcare systems in the United States, Delaware based ChristianaCare is home to a wide variety of medical experts. Now live, the ChristianaCare Speakers Bureau features 80 experts who are currently available for speaking engagements on a wide variety of health topics including: Aging and Senior Health, Cancer, Children’s Health, COVID-19, Diabetes, Pregnancy and Childbirth. Sports Medicine, Stroke, Weight Management and Women’s Health. Designed with the ExpertFile platform, the ChristianaCare Speakers Bureau provides easy discovery and access to experts, including their biographies, downloadable photographs, samples of past presentations, languages spoken and more. The site can be viewed here. Screenshot from the new ChristianaCare Speakers Bureau launched Aug. 2023. The site provides easy discovery and access to experts, with the ability to search by topics and keywords. Detailed profiles for experts include biographies, downloadable photographs, samples of past presentations, languages spoken and more. How a Speakers Bureau boosts thought leadership A Speaker's Bureau is an initiative within an organization that assembles a team of expert speakers who can represent the organization and speak authoritatively on its behalf. While media appearances are often the core focus for experts in organizations, a Speakers Bureau opens up additional opportunities to speak at events such as in-person conferences, webinars, podcasts. Speakers ideally represent a diverse group of professionals from within the organization, and can share their knowledge, insights, and experiences on a range of topics relevant to the organization's mission, values, and field of work. Through event appearances, these experts help to enhance the organization's visibility, foster community engagement, and solidify the organization's reputation as a thought leader in its field. Speakers Bureaus provide effective and efficient way to promote the organization's initiatives, achievements, and viewpoints to the wider public. Creating New Connections Between Experts and the Community Following a string of successes that followed the launch of their ChristianaCare Experts site that resulted in major increases in national media coverage and SEO performance, the formation of a Speakers Bureau was a smart move that will further extend the reach of the ChristianaCare brand. Events provide an excellent way to connect meaningfully with a wider audience to help ChristianaCare make progress on key goals such as delivering effective community health education and improving healthcare equity. “At ChristianaCare, our mission of service to the community includes a commitment to provide timely, accurate health information so that people can make informed decisions about their health,” said Karen Browne, vice president of marketing and communications. “Through our new speakers bureau, we’ve expanded our capacity to meet these needs in the community.” The Benefits of a Speakers Bureau Given the fragmentation of traditional media channels and the massive growth in events such as webinars and podcasts, Speakers Bureaus are fast gaining popularity as a proven way to personify your organization and build a stronger connection to your brand. So far the ChristianaCare Speakers Bureau appears to be off to a solid start. "We had a huge response to our media release when we launched earlier this week and in the first day alone we had multiple organizations sending speaking opportunities for our medical experts. We're also seeing a great response internally as more of our experts requested to join the Speakers Bureau once it went live," said Hiran Ratnayake, Senior Manager of Media Relations at ChristianaCare who played a key role in developing the Speakers Bureau with his colleagues Shane Hoffman, Communications Director and Tom Hendrich - Senior Digital Content Editor at ChristianaCare. Is a Speakers Bureau Right For Your Organization? Here are some key benefits to consider in determining if a speakers bureau makes sense for your organization: Bolsters Community Engagement: An active Speaker's Bureau helps create a bridge between your organization and the community you serve. Promotes Diversity and Inclusion: A Speaker's Bureau offers an exciting opportunity to showcase the diverse voices and unique experiences within your organization. Enhances Organizational Visibility: The increased exposure at events can lead to greater recognition in the industry, more opportunities for collaborations, and ultimately, a wider reach for your healthcare services. It also is a proven way to boost SEO pagerank and domain authority in search engines and also provides a lot of additional content for your social channels. Develops Professional Skills: For healthcare professionals who participate, a Speakers Bureau offers an excellent opportunity to develop public speaking skills, foster leadership abilities, and establish themselves as thought leaders in their respective fields. Facilitates Knowledge Sharing: A Speaker's Bureau cultivates a more dynamic learning environment, which can lead to new ideas, innovations, and improved patient care within your organization. Strengthens Crisis Management Readiness: Having a pool of trained speakers ready to contribute can be incredibly beneficial in times of crisis. These professionals can help your communications team more effectively communicate critical information to the public, media, and other stakeholders. Enhances Employee Engagement: Employees who are given the opportunity to share their knowledge and represent their organization publicly, often feel more valued and invested in their work. Going Beyond the Walls of Your Medical Facility In the constantly evolving world of healthcare, accurate and timely information is critical to informed patient decisions and effective treatments. Organizations such as ChristianaCare understand that their role as a prominent healthcare system is to deliver information that extends beyond their immediate medical responsibilities. It’s simply no longer adequate to provide care within the walls of a medical facility. Today there is a critical demand for a more engaged approach, requiring hospitals and healthcare systems to leverage their in-house expertise for community education. A more informed community, armed with knowledge, which can make empowered decisions about their healthcare. While the public has an abundance of medical information at their fingertips, to help them participate more actively in their healthcare, much of the information found on social media today often lacks clarity, context, and credibility, leading to confusion and misinterpretations. Healthcare experts, leaders, and executives can play a pivotal role in dispelling myths and offering credible, evidence-based insights. An engaged, approachable healthcare professional is a reassuring sight, reinforcing the community’s faith in the system. It’s a win-win for these experts and the healthcare institution they represent. And most importantly it's a win for the communities they serve, as people identify potential health issues earlier, adopt healthier lifestyles, and reduce emergency hospital visits. This puts less burden on the region’s healthcare system, and better utilizes resources to reach a broader audience. After all, healthcare is not just about curing the sick; it’s about educating, engaging, and empowering the community for a healthier future. Congratulations to the entire team at ChristianaCare for creating such a valuable resource for your community. And thank you for letting us be a part of this exciting journey.

#Expert Insight: Let’s Talk About Maternal and Postpartum Health
With increased maternal mortality rates in the news, and births involving inductions and c- sections on the rise despite their risks, Elizabeth Johnson-Young asks: 'What communication choices and strategies do women use after a negative birth experience?' Many women define certain aspects of childbirth as traumatic – from a mother or child’s life being put at risk to a host of less serious circumstances that can cause an unfavorable natal experience – and that can pose a threat to mental health. Who will they trust next when it comes to their maternal healthcare and their future decisions regarding birth? Johnson-Young’s project, “Birth, Trauma, and Communicating Maternal Health,” uses in-depth interviews of women who define their birth experience as difficult or traumatic. It focuses on choices and perceptions, and discusses the potential outcomes of listening, language and support. This is an important topic for health care providers, families and mothers and if you are looking to know more - then let us help. Dr. Elizabeth Johnson-Young is a published expert on health communication, especially maternal and family health. She is ready to help if you are looking to cover this topic - simply click on her icon now to arrange an interview today.

Ana Palacios’ interview on “Eagle Eye View,” the official podcast of Georgia Southern University. Palacios discusses her research and how being a mom motivated her. Several esteemed nutrition researchers collaborated on “Effectiveness of Lactation Cookies on Human Milk Production Rates: A Randomized Controlled Trial,” which was recently published in The American Journal of Clinical Nutrition. David B. Allison, Ph.D., dean of the Indiana University School of Public Health-Bloomington (SPH-B), is among the researchers who conducted a one-month, randomized controlled trial of lactating parents of healthy babies in the same age range. Their findings revealed no evidence for an effect of consuming lactation cookies on human milk production. “Too often in the field of nutrition and food, strong beliefs—sometimes even well-reasoned conjectures based upon some scientific knowledge—are mistaken for demonstrated facts,” Allison said. “Conjecture is good, but knowing is better. We come to know about the effects of nutrition and dietary supplements through rigorous, randomized, controlled trials. Having conducted such a study on lactation cookies, we found no evidence for their effectiveness. “This does not mean that it is impossible for any lactation cookie to affect human milk production,” he continued. “This study does suggest that the cookies we studied—under the conditions we studied them—have no discernible effect. The burden of proof seems to now be on those who claim there is an effect.” The study followed 176 U.S. parents who were exclusively breastfeeding healthy two-month-old babies. One group of parents was provided a serving of commercially available lactation cookies to consume daily for a month; the other group of parents ate a serving of conventional cookies not designed to increase lactation, each day for a month. Through a weekly survey, parents reported the quantity of milk they produced after following a validated milk expression protocol using a hospital-grade breast pump, providing data that were analyzed by both the study authors and an independent statistician. These data demonstrated that the impact of consuming lactation cookies did not have a significant effect on how much milk was actually produced or perceived to be produced by the lactating parents. The authors assert that consumers should be cautious when considering the potential effect of this product, or any food and/or supplement that promotes health-promoting benefits without published, peer-reviewed scientific evidence to support its claims. As the researchers noted, these lactation cookies can contain substantial calories and sugars, which could affect postpartum weight loss efforts and related health issues. “Despite being a physician and nutrition scientist focused on early-life nutrition, I still remember how difficult breastfeeding was for me with both of my children,” said study lead author Ana M. Palacios, MD, Ph.D., assistant professor, Department of Health Policy and Community Health, Jiann-Ping Hsu College of Public Health at Georgia Southern University. “Our research highlights that lactation cookies, which include added sugars and saturated fat, may not have the said purported benefits of increasing milk production. Purchasing lactation cookies to increase milk production may pose an unnecessary cost and may have additional implications for parents, such as limiting post-pregnancy weight loss and reducing consumption of healthier foods. More research is needed to better understand what foods and nutrients can best help increase milk supply in diverse populations.” The full article, along with the list of contributing authors, is available by simply clicking the article below: Interested in learning more? For more information about this research or to speak with Ana M. Palacios — simply reach out to Georgia Southern's Director of Communications Jennifer Wise at jwise@georgiasouthern.edu to arrange an interview today.
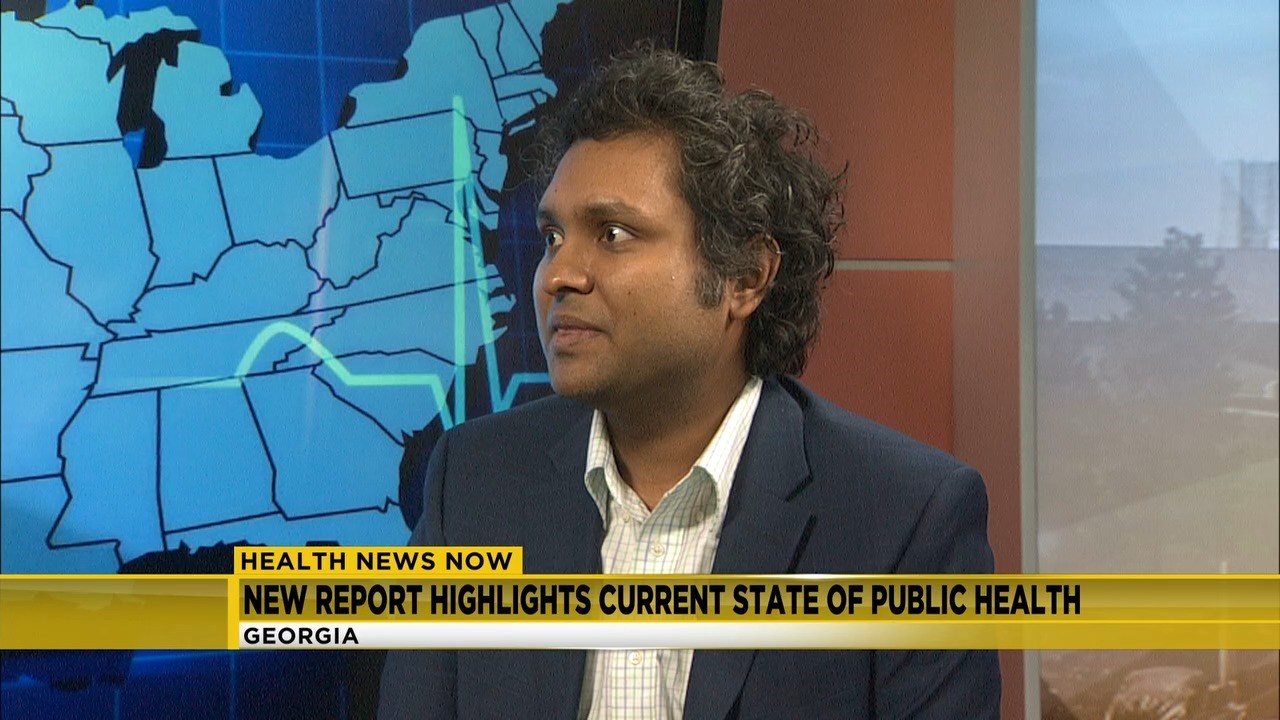
Augusta University’s second annual Healthy Georgia Report has been released, offering a snapshot of health in the Peach State as compared to not only neighboring states, but also the entire country. While Georgia’s population is doing well in some key health factors, researchers also found areas that could benefit from more awareness and public policy action. Biplab Datta, PhD, assistant professor in the Institute of Public and Preventive Health and the Medical College of Georgia’s Department of Population Health Sciences, collaborated with other IPPH faculty and staff to update the report and add new categories this year. The goal of the report is to connect with lawmakers, community leaders and researchers, stimulate conversations about public health needs and promote action, such as greater community engagement, research for informing effective policies and appraisal of required funds. “We need to make lawmakers aware of the public health situation in the state of Georgia,” said Datta. “We hope this report will help identify areas that need policy attention. It can also play an important role in bridging the gap between researchers and policymakers.” Using 2021 data from the Behavioral Risk Factor Surveillance system, the National Survey of Children’s Health, the American Community Survey and the Center for Disease Control and Prevention’s COVID Data Tracker website, the report was compiled on numerous health topics. Some categories studied include high cholesterol, hypertension, obesity, arthritis, asthma, cancer, cardiovascular diseases, alcohol consumption, diabetes and more. It also broke down each category by age, sex, race, income level and other socioeconomic indicators to get a full representation of the data. New to the study this year is an in-depth look at health insurance coverage, COVID-19 vaccinations, breastfeeding, child maltreatment, and unmet healthcare need of children. Georgia ranks 49th in the nation when it comes to health insurance coverage. That was a surprise to Datta. “I didn’t expect the numbers to be that bad, but I think it also indicates the scope of work that we need to undertake to improve insurance coverage in Georgia,” he said. Another surprise was the low rate of flu vaccination in Georgia. “We know there is a difference between whites and Blacks in the U.S. But when we look at and compare Black people in Georgia with Blacks in the rest of the southeastern states, we see the flu vaccination rate was significantly lower among Blacks in Georgia. This is an issue that warrants further research to understand the underlying causes of such disparity,” said Datta. As it was a year ago, hypertension remains a concern. There are several issues involved when talking about hypertension but there are also straightforward ways to improve the condition Datta said. “I think one of the core components of hypertension control is just changing some behavioral stuff. If we just reduced the sodium content in our daily diet, if we do regular physical exercise for a certain amount of time that will significantly improve our hypertension management. Community-level initiatives to make people aware of these things can make a real difference,” said Datta. Residents in Georgia are doing better in several areas such as obesity, cancer rates, asthma prevalence and depressive disorders. Datta said it’s important to recognize these improvements so we can learn from them. “We need to figure out where we are doing well and use that experience in areas where we are not doing so well. It will help us move toward the right direction.” He added it’s important to always be looking for ways to evolve the study, and that includes adding new categories when enough data is available. “We didn’t cover sexually transmitted diseases in this year’s report, which we would like to add when data will become available. We’d also like to add teenage pregnancy, maternal health issues, gun violence and opioid use,” he said. Looking to learn about health in the Peach State? Then let us help. Biplab Datta is available to speak with media regarding this important topic. Simply click on his icon now to arrange an interview today.

ChristianaCare Rated a High Performing Hospital for Maternity by U.S. News & World Report
ChristianaCare is the only health system in Delaware to earn the High Performing designation from U.S. News ChristianaCare has earned the highest award for maternity care that a hospital can achieve from U.S. News & World Report in its 2022-23 ratings for Best Hospitals for Maternity Care. Rated as a High Performing Hospital, ChristianaCare was the only health system in Delaware to earn this esteemed honor. Christiana Hospital at ChristianaCare’s Newark Campus is the only high-risk delivering hospital in the First State offering Level III neonatal intensive care. More than 6,100 babies are born at Christiana Hospital each year. The U.S. News Best Hospitals for Maternity Care methodology is based entirely on objective measures of quality, such as C-section rates in lower-risk pregnancies, newborn complication rates, exclusive breast milk feeding rates, early elective delivery rates and vaginal birth after cesarean (VBAC) rates, among other measures. “When we announced plans seven years ago to build the ChristianaCare Center for Women’s & Children’s Health, we affirmed our commitment to provide superior-quality care for women and infants in our region,” said Matthew Hoffman, M.D., MPH, FACOG, Marie E. Pinizzotto, M.D., Endowed Chair of Obstetrics and Gynecology at ChristianaCare. “This prestigious recognition is an affirmation that patients who choose to give birth at ChristianaCare will have access to the very best services and expertise to ensure a safe delivery and a healthy baby.” Just two years ago ChristianaCare opened the Center for Women’s & Children’s Health, an eight-story, approximately 400,000-square-foot tower at Christiana Hospital. The center uses the most up-to-date, evidence-based models of care, with improved integration of services and the space to offer innovative patient-centered care for mothers, babies and families. One of the most significant features of the new center is a state-of-the-art neonatal intensive care unit (NICU), featuring private rooms with sleep-in space for families. Christiana Hospital is one of the only hospitals in the United States to provide “couplet care” in the NICU, keeping the mother and baby together even if they both require medical care. This is based on a European model demonstrating that moms are more likely to breastfeed in this environment, which is particularly important in the early development of children. “We best achieve optimal health and flourish when we are able to begin our lives as healthy newborns,” said David Paul, M.D., chair of ChristianaCare’s Department of Pediatrics. “Building this transformative women’s and children’s hospital was a way to invest in the future of our community’s children. In addition to our outstanding caregivers and the care we provide within the walls of the hospital, this facility is a monumental step forward in enabling us to care for moms and babies, and we are delighted that U.S. News has recognized what a special place it is.” Other innovative features at the center include: Expanded labor and delivery suites. Private rooms for mothers and families after delivery. A spacious, multi-level Ronald McDonald Family Room to support families with infants who are in intensive care. Expanded OB/GYN emergency services area and new labor lounge. Separate admitting and discharge areas for the convenience of our patients. A tranquil family rooftop garden that provides spaces for play and relaxation. Vibrant sibling play spaces with interactive displays and artwork, and open community spaces for health education and programs. U.S. News’ annual evaluation is designed to assist expectant parents and their doctors in making informed decisions about where to receive maternity care. U.S. News evaluated nearly 650 hospitals that provide high-quality labor and delivery services for uncomplicated pregnancies for its 2022-2023 Best Hospitals for Maternity Care. Fewer than half of all hospitals that offer maternity care and participated in the survey received a High Performing designation. “When expectant parents are considering their options for welcoming a baby to the world, the Best Hospitals for Maternity Care are designed to help them identify hospitals that excel in delivering babies for uncomplicated pregnancies,” said Ben Harder, chief of health analysis and managing editor at U.S. News & World Report. “A hospital that has earned a High Performing designation may be a good option for parents, in consultation with their medical provider, to consider.” Excellence in Maternity Care Built on Experience and Research ChristianaCare’s Center for Women’s & Children’s Health includes Delaware’s most experienced maternity team, and it is also a significant research institution. Since opening, the Center for Women’s & Children’s Health participated in a significant study that found that treating mild chronic hypertension with medications is beneficial and safe for mother and baby. Published in The New England Journal of Medicine, the world’s foremost medical journal, the study has the potential to change the standard of care for some pregnant women, as it represented the first time that comprehensive, evidence-based data showed the benefits of treating mild forms of chronic hypertension during pregnancy. “Our commitment to research is a path to better caring for our community,” said Dr. Hoffman, a co-author in the study. About ChristianaCare Headquartered in Wilmington, Delaware, ChristianaCare is one of the country’s most dynamic health care organizations, centered on improving health outcomes, making high-quality care more accessible and lowering health care costs. ChristianaCare includes an extensive network of primary care and outpatient services, home health care, urgent care centers, three hospitals (1,299 beds), a freestanding emergency department, a Level I trauma center and a Level III neonatal intensive care unit, a comprehensive stroke center and regional centers of excellence in heart and vascular care, cancer care and women’s health. It also includes the pioneering Gene Editing Institute. ChristianaCare is nationally recognized as a great place to work, rated by Forbes as the 2nd best health system for diversity and inclusion, and the 29th best health system to work for in the United States, and by IDG Computerworld as one of the nation’s Best Places to Work in IT. ChristianaCare is rated by Healthgrades as one of America’s 50 Best Hospitals and continually ranked among the nation’s best by U.S. News & World Report, Newsweek and other national quality ratings. ChristianaCare is a nonprofit teaching health system with more than 260 residents and fellows. With its groundbreaking Center for Virtual Health and a focus on population health and value-based care, ChristianaCare is shaping the future of health care.

Preterm Birth and Lifelong Health
November is Prematurity Awareness Month—a month that places a spotlight on the current state of maternal and infant health in the United States and globally. According to the nonprofit March of Dimes, one in 10 babies is born preterm each year in the U.S. But what does that mean, and why do we need to consider gestation period post-birth? We sat down with Michelle Kelly, PhD, CRNP, CNE, FAANP, associate professor of nursing at Villanova University's M. Louise Fitzpatrick College of Nursing, to discuss and explain the importance of preterm education for lifelong health. Q: To begin, what qualifies as preterm birth? Dr. Kelly: A full-term pregnancy lasts 40 weeks. Infants born before the completion of 37 weeks of gestation are preterm. And there are levels of prematurity: Extremely preterm: Infants born before the completion of 25 weeks of gestation. Very preterm: Infants born before the completion of 32 weeks of gestation. Moderately preterm: Infants born between 32-34 weeks of gestation. Late preterm: Infants born between 34-36 weeks of gestation. Q: Why do health practitioners need to be aware of gestation history? DK: Understanding the potential long-term physical and mental health implications is essential to mitigating the risks. Clinicians cannot change the reality that someone was born early. However, clinicians can utilize that information in treatment decisions. Instituting treatment or therapies early can help minimize the expression of that risk and improve future health. Q: What are the health risks for children born prematurely? DK: The earlier an infant is born, the greater the risk to their overall health and development. And while it is much better to be born at 35 weeks instead of 25 weeks, it does not mean that those born closer to term escape all risks. During infancy and childhood, a preterm birth can cause difficulty with breathing, feeding, gaining weight appropriately and achieving important developmental milestones. Research suggests that children and adolescents born at any level of prematurity are at risk for challenges in school, conditions that require physical or behavioral therapy as well as conditions typically associated with immature body systems, such as respiratory issues like asthma. Additionally, long-term follow-up studies indicate that risk continues into adolescence and adulthood. Q: What are some long-term issues that stem from being born preterm? DK: Adolescents and adults born preterm continue to be at risk for reduced lung function, wheezing and asthma. Research findings suggest that there are also cardiovascular risks, particularly an increased incidence of hypertension (high blood pressure). Additionally, an increased incidence of mental health conditions, specifically anxiety and depression, are associated with preterm birth. All these increased risks are modifiable with early recognition and treatment. Q: What recent research has been conducted and what strides have been made to improve the lives of those born preterm? Is the prognosis for those born preterm positive? DK: Today's NICU environment is vastly different from the NICU of the past. Premature babies born in the last 20 years have survival rates that exceed 95 percent for all but the earliest of gestational ages. Increased attention to developmentally supportive care, breastfeeding, kangaroo care and the recognized importance of family presence in the NICU is now the standard of care. Research and advocacy aimed at supporting families touched by prematurity and raising awareness of healthcare providers and K-12 educators are gaining international attention. While being born preterm presents lifelong risks, identifying and communicating one's status with health practitioners early and often allows for effective treatment and positive outcomes.








